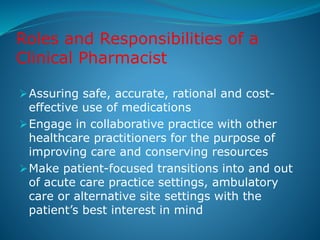
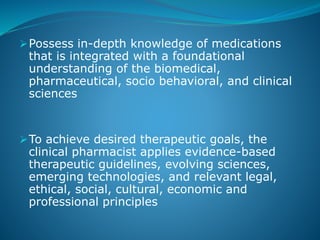
Clinical pharmacy involves applying scientific principles of pharmacology to optimize patient care and outcomes. It focuses on rational medication use and promoting health. Clinical pharmacists work directly with patients, assessing their medication-related needs and developing individualized care plans in collaboration with other healthcare providers. They are highly trained and educated professionals responsible for ensuring safe, effective, and cost-efficient use of medications across various healthcare settings.