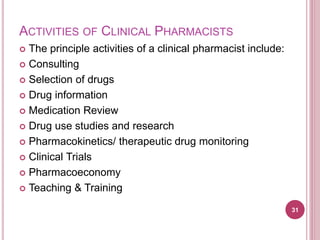
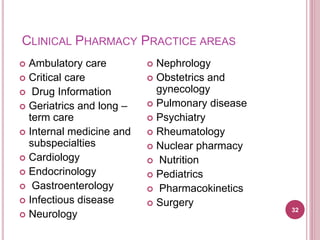
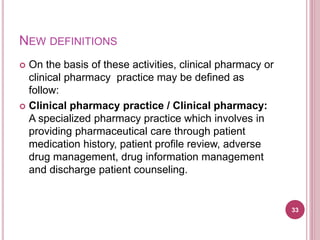
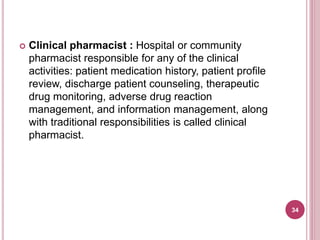
Clinical pharmacy involves optimizing medication use for patients and promoting health. It focuses on applying pharmacists' expertise with pharmaceuticals to directly improve patient care. Historically, clinical pharmacy emerged in response to drug-related issues in the 1960s. A clinical pharmacist's role includes activities like medication management, patient education, and adverse drug reaction monitoring to develop individualized care plans with the healthcare team. The overall goal is to maximize the benefits and minimize the risks of drug therapy for each patient.