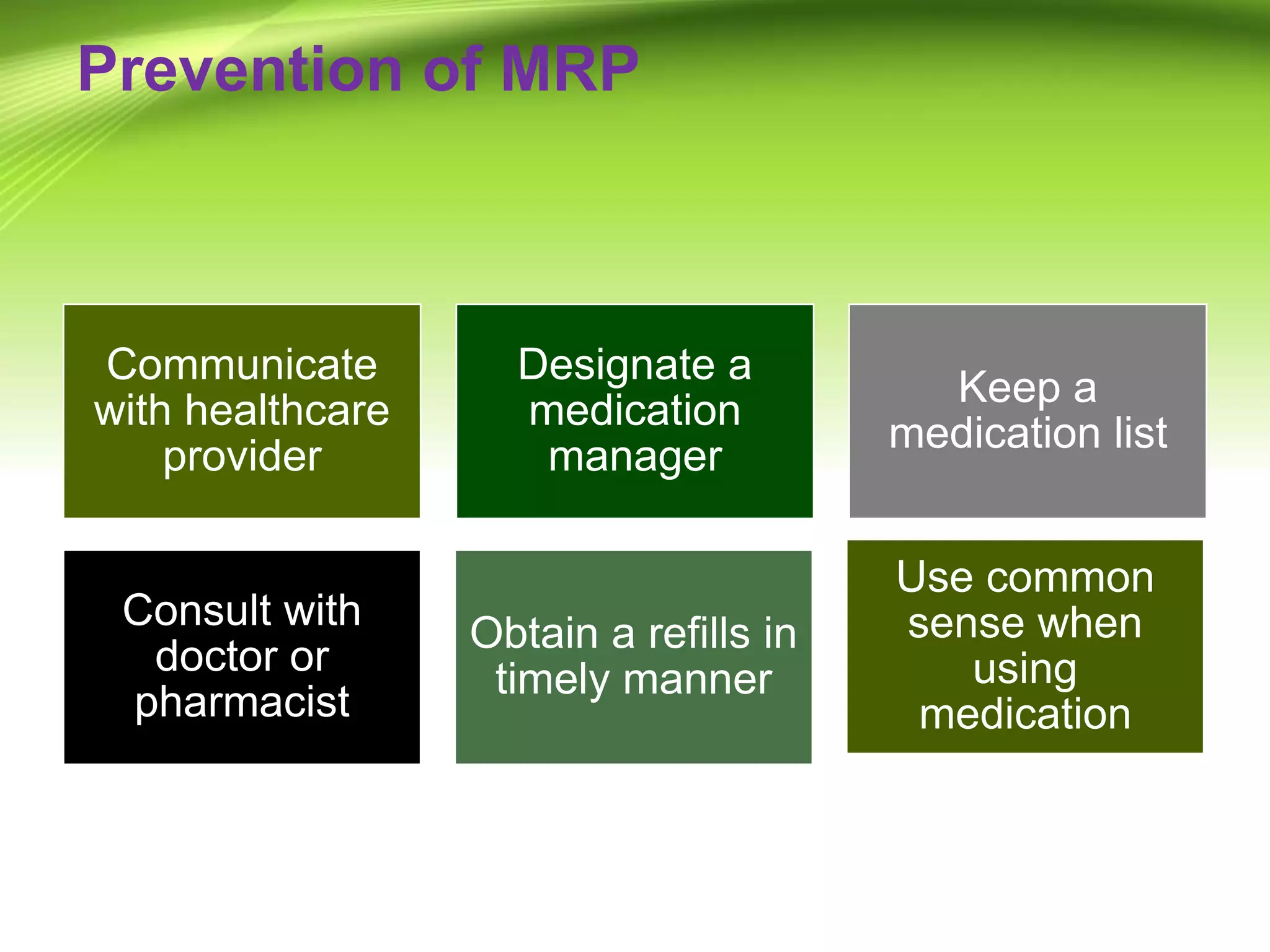
The document outlines the role and responsibilities of clinical pharmacists, emphasizing their engagement in patient care, medication management, and collaboration with healthcare teams. It distinguishes clinical pharmacy from traditional pharmacy by focusing on individual patient needs and the safe use of medications. Key components include assessing medication requirements, monitoring drug efficacy, and providing patient education.