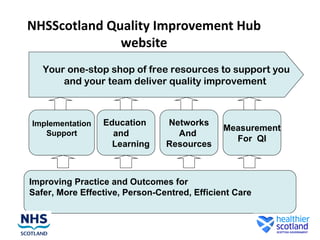
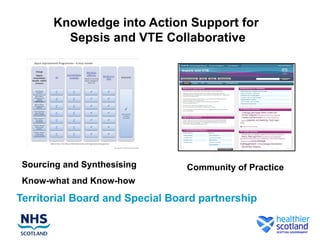
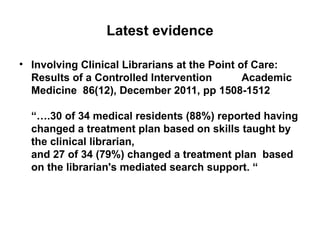
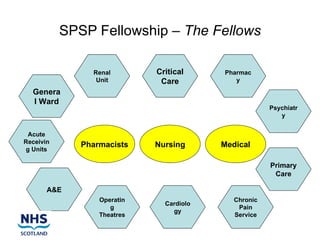
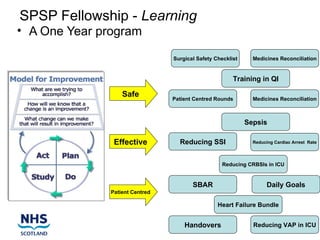
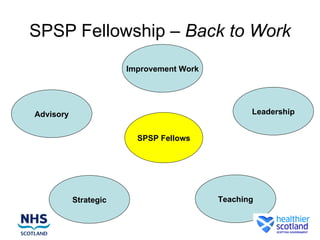
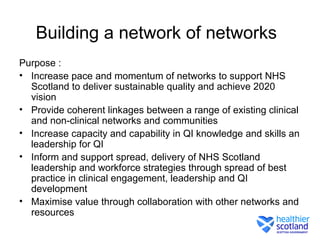
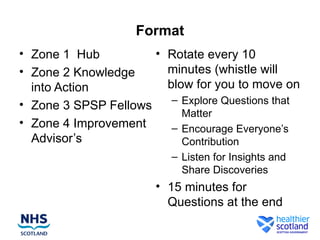
This document summarizes resources from the Quality Improvement Hub in Scotland. It describes the hub's website as a one-stop shop for free quality improvement resources. It outlines support available for implementation, education, networks, and measurement. It also summarizes programs for a Quality Improvement Education Program, Knowledge into Action initiative, SPSP Fellowship, and building a network of networks to spread best practices in healthcare quality improvement across Scotland.