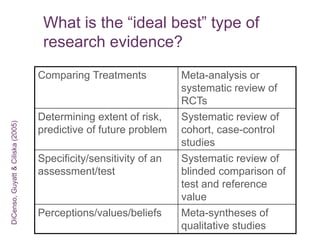
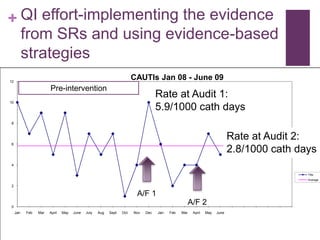
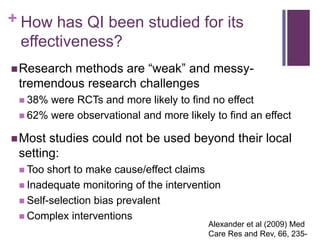
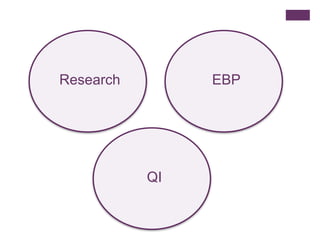
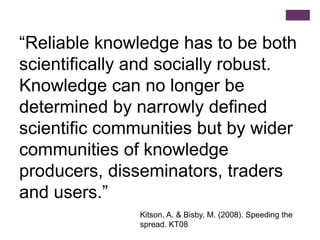
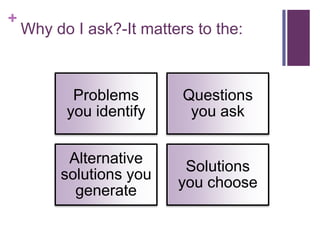
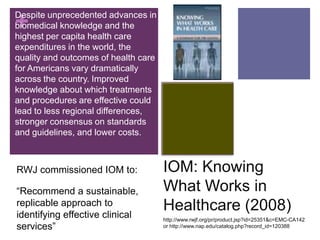
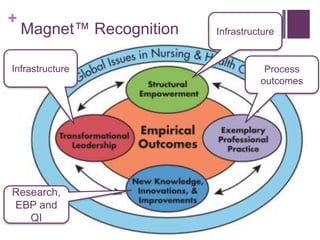
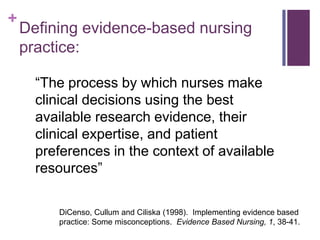
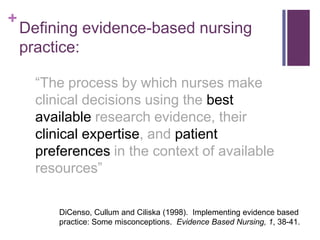
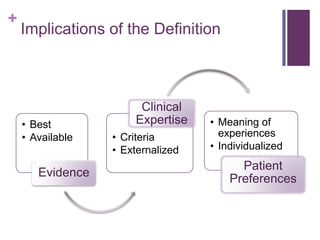
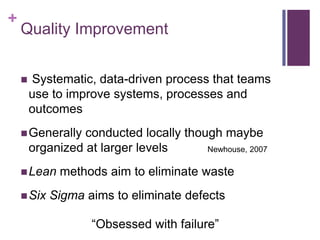
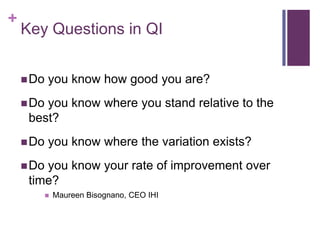
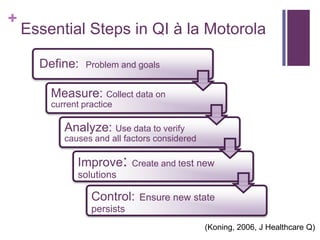
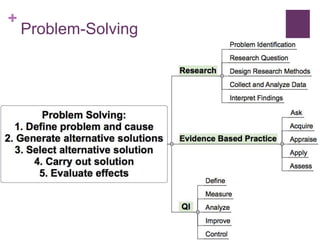
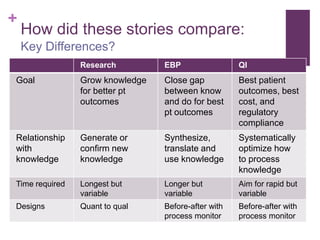
This document discusses the distinctions, synergies, and infrastructures needed to optimize patient outcomes through evidence based practice, research, and quality improvement. It compares the problem solving processes of quality improvement, evidence based practice, and clinical research. Quality improvement uses a systematic, data-driven approach to improve processes and outcomes, while evidence based practice involves using the best available research evidence, clinical expertise, and patient preferences to make decisions. Clinical research aims to generate generalizable knowledge through systematic study and evaluation. Infrastructure characteristics like mentorship, leadership, and culture can promote high quality outcomes, evidence uptake, and clinical inquiry.




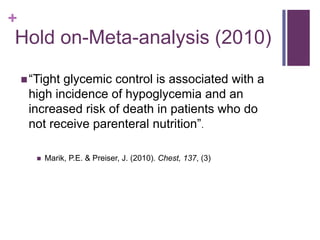
![+ Hold on-Meta-analysis (2010)
7 RCTs pooled with 11,425 pts
IITdid not:
Reduce 28-day mortality (OR=.95 [CI, .87-
1.05]
Reduce BSI (OR=1.04 [CI, .93-1.17]
Reduce renal replacement tx (OR=1.01 [CI,
.89-1.13]
IITdid:
Increase hypoglycemic incidents (OR=7.7
[CI, 6.0-9.9] Marik, P.E. & Preiser, J. (2010).
Chest, 137, (3)](https://image.slidesharecdn.com/qiebpresearch-121213140913-phpapp02/85/Qiebp-research-56-320.jpg)
![+ Hold on-Meta-analysis (2010)
Meta-regression revealed:
Relationship between proportion of parenteral
calories and 28-day mortality
Leuven trials tx effect related to parenteral feeding
Harm?
Mortalitylower in control (glc 150 mg/dl) OR=.9 [CI,
.81-.99] when Leuven trials removed
Noevidence to support IIT in general med-
surg ICU pts fed according to current
guidelines (ie, enteral) Marik, P.E. & Preiser, J. (2010).
Chest, 137, (3)](https://image.slidesharecdn.com/qiebpresearch-121213140913-phpapp02/85/Qiebp-research-57-320.jpg)