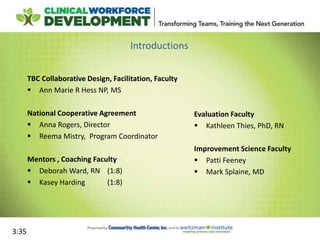
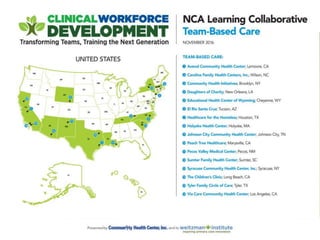
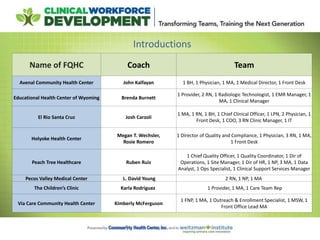
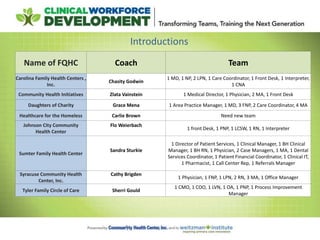
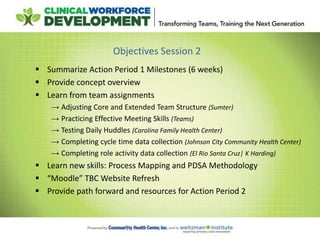
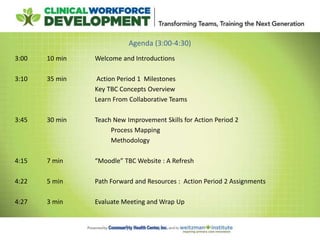
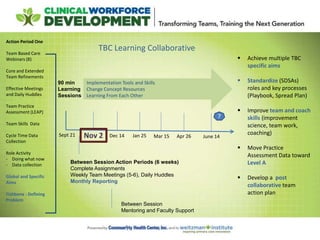
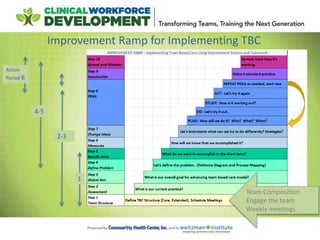
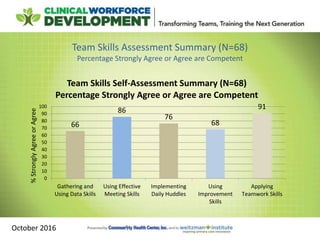
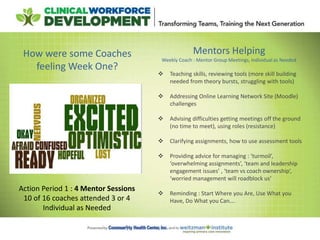
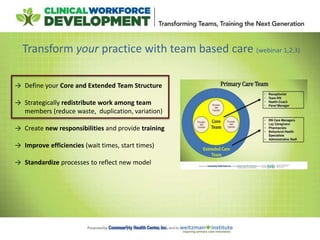
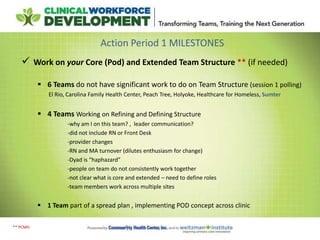
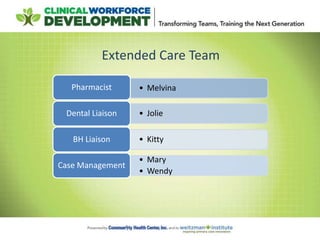
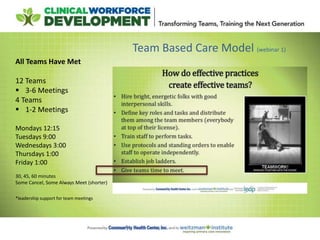
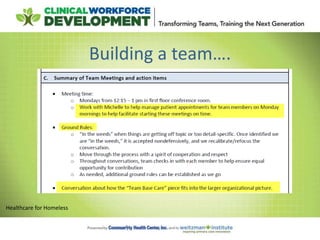
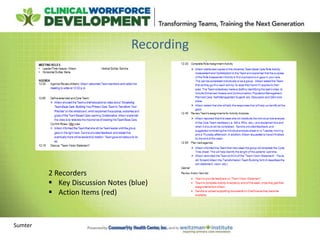
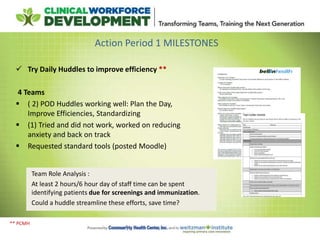
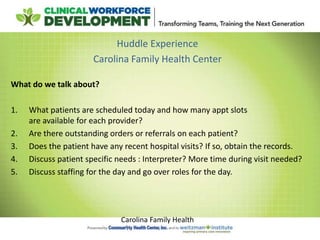
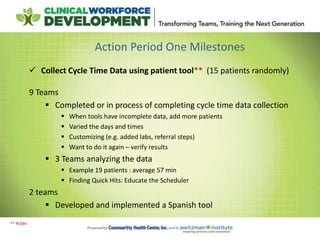
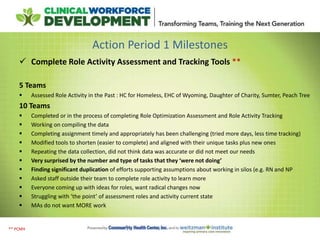
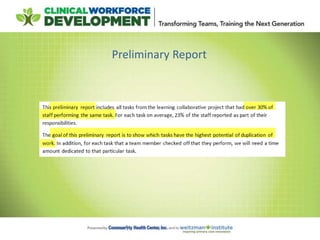
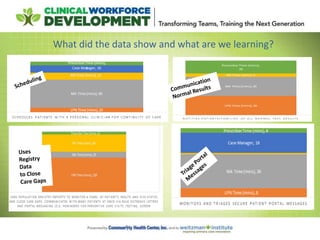
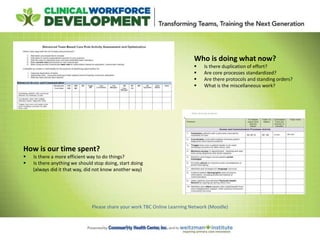
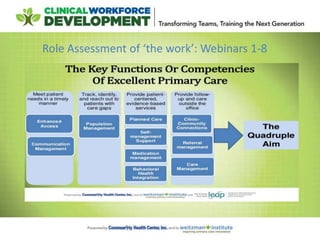
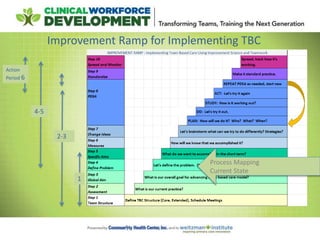
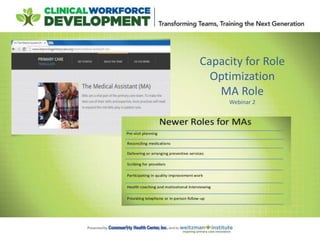
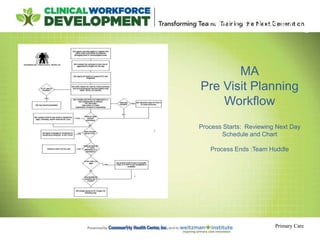
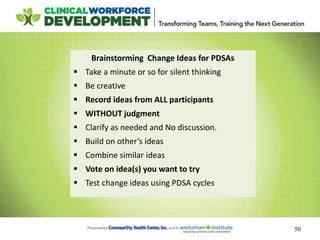
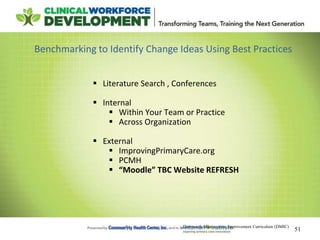
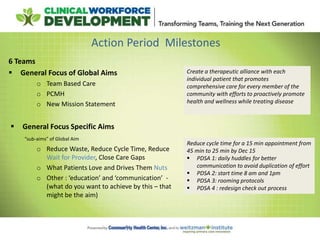
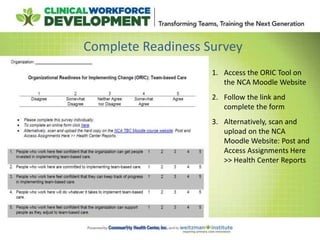
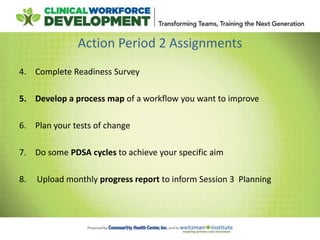
This document provides an agenda and notes for a session of the Team Based Care Learning Collaborative. The session began with introductions of participating teams and their members. Teams then shared their experiences implementing various aspects of team-based care over the past six weeks, including adjusting team structures, practicing effective meeting skills, testing daily huddles, collecting data, and refining roles. New improvement skills and methodology were taught, including process mapping and the PDSA cycle. Teams received guidance on next steps and were assigned tasks for the coming period to continue working to implement team-based care models in their practices.