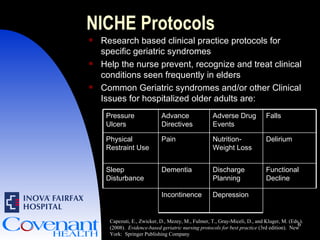
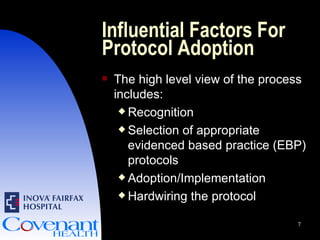
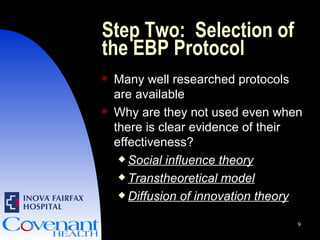
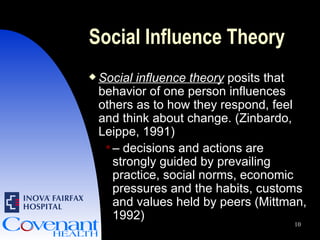
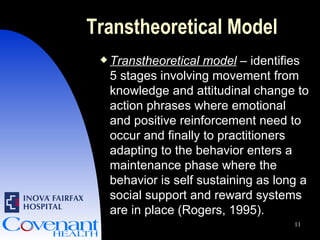
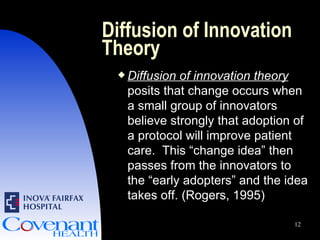
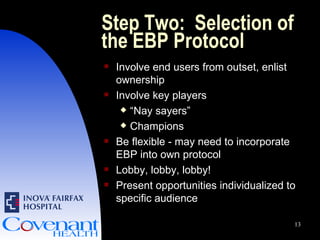
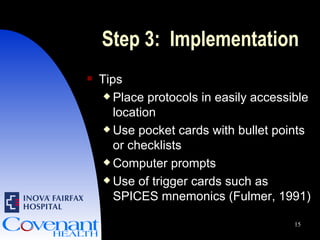
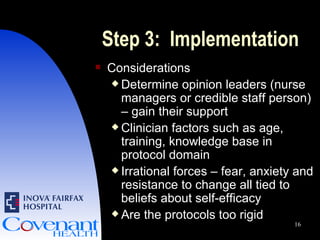
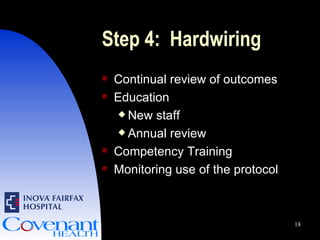
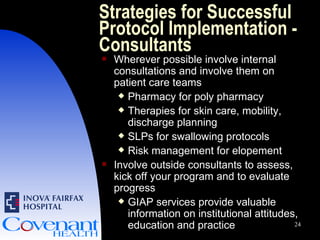
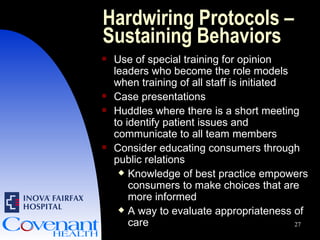
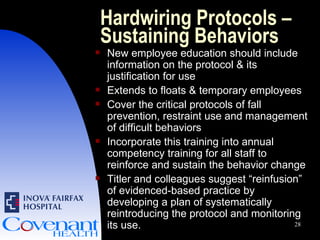
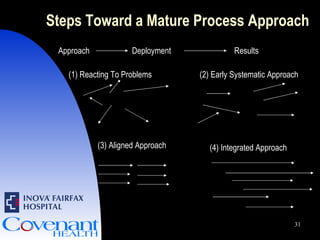
This document discusses factors to consider when developing and implementing clinical protocols for older adult patients. It outlines a 4-step process: 1) recognizing areas for improvement, 2) selecting evidence-based protocols, 3) implementing protocols through strategies like education and hardwiring into documentation, and 4) measuring performance through reliable tools. Interprofessional collaboration and support from administrators are also emphasized as key to successful protocol adoption.