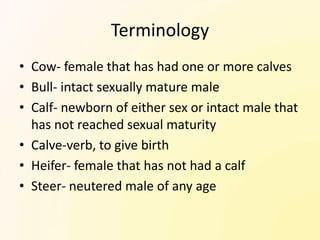
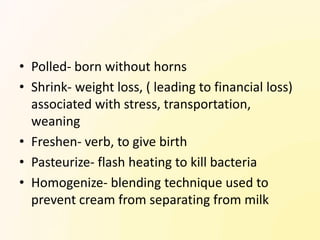
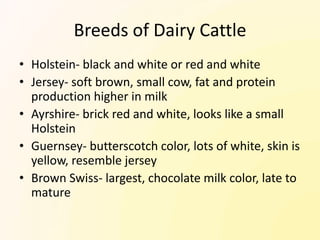
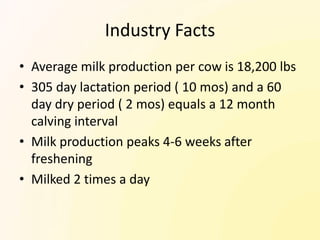
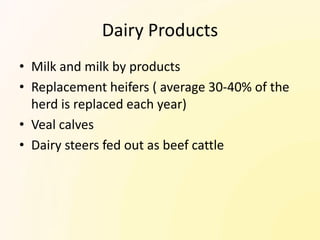
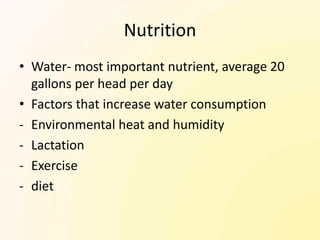
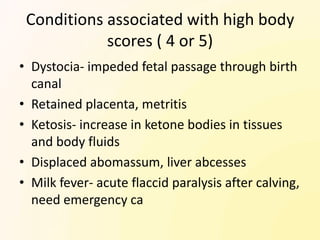
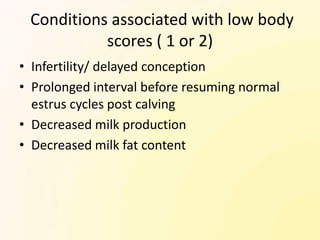
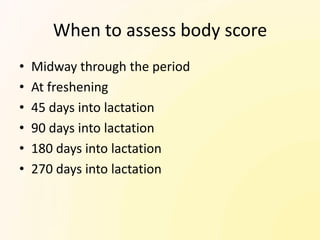
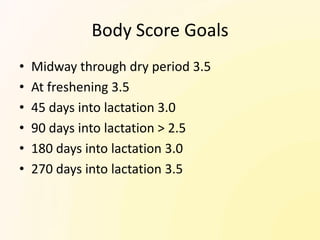
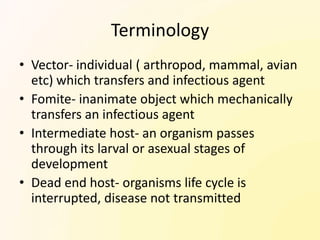
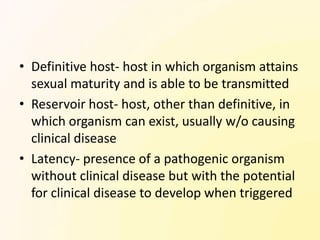
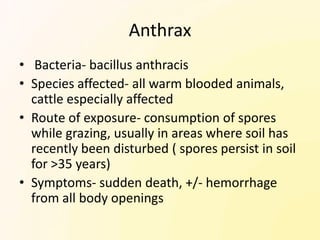
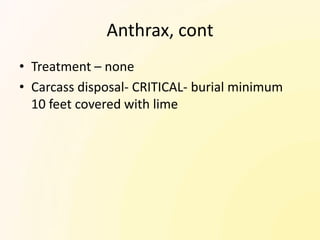
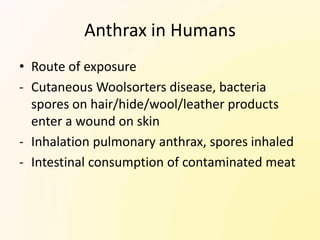
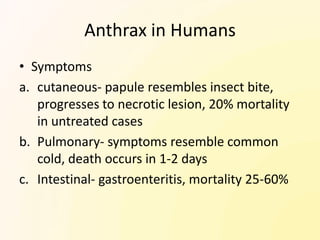
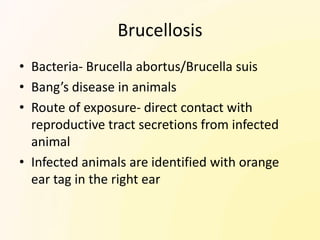
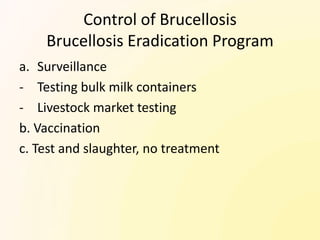
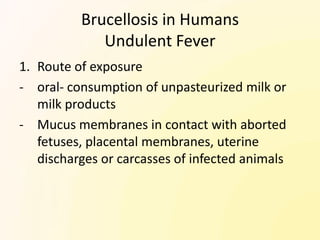
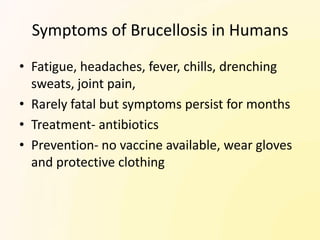
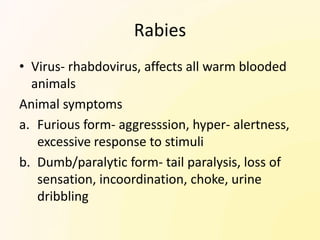
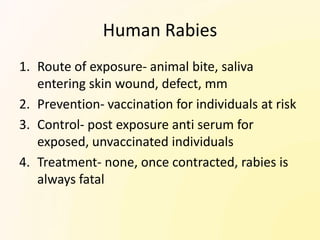
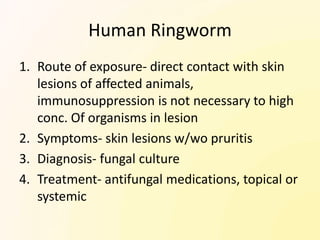
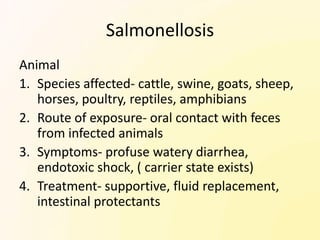
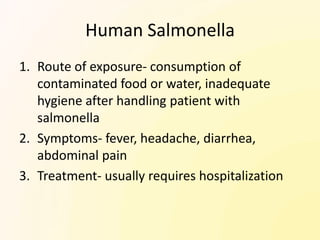
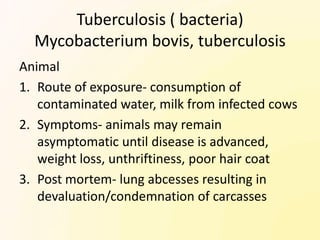
Dairy cattle terminology and industry facts were provided. Key points included definitions of terms like cow, bull, calf and heifer. The average milk production per cow is 18,200 lbs over a 305 day lactation period. Main dairy breeds discussed were Holstein, Jersey, Ayrshire and Guernsey. Body condition scoring was also summarized to monitor cow health and productivity. Several zoonotic diseases transmissible from cattle to humans like anthrax, brucellosis, rabies, ringworm and salmonellosis were outlined.