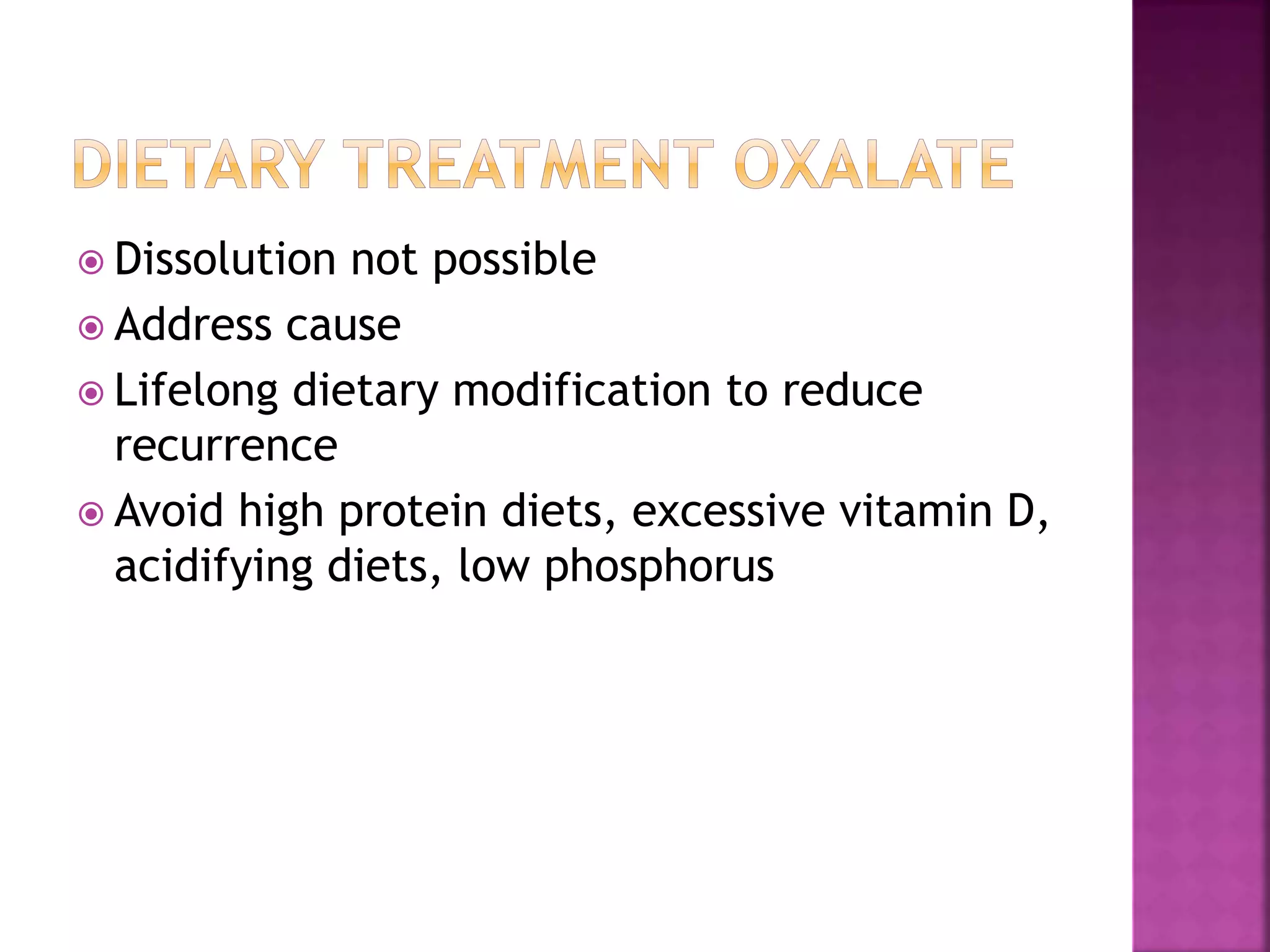
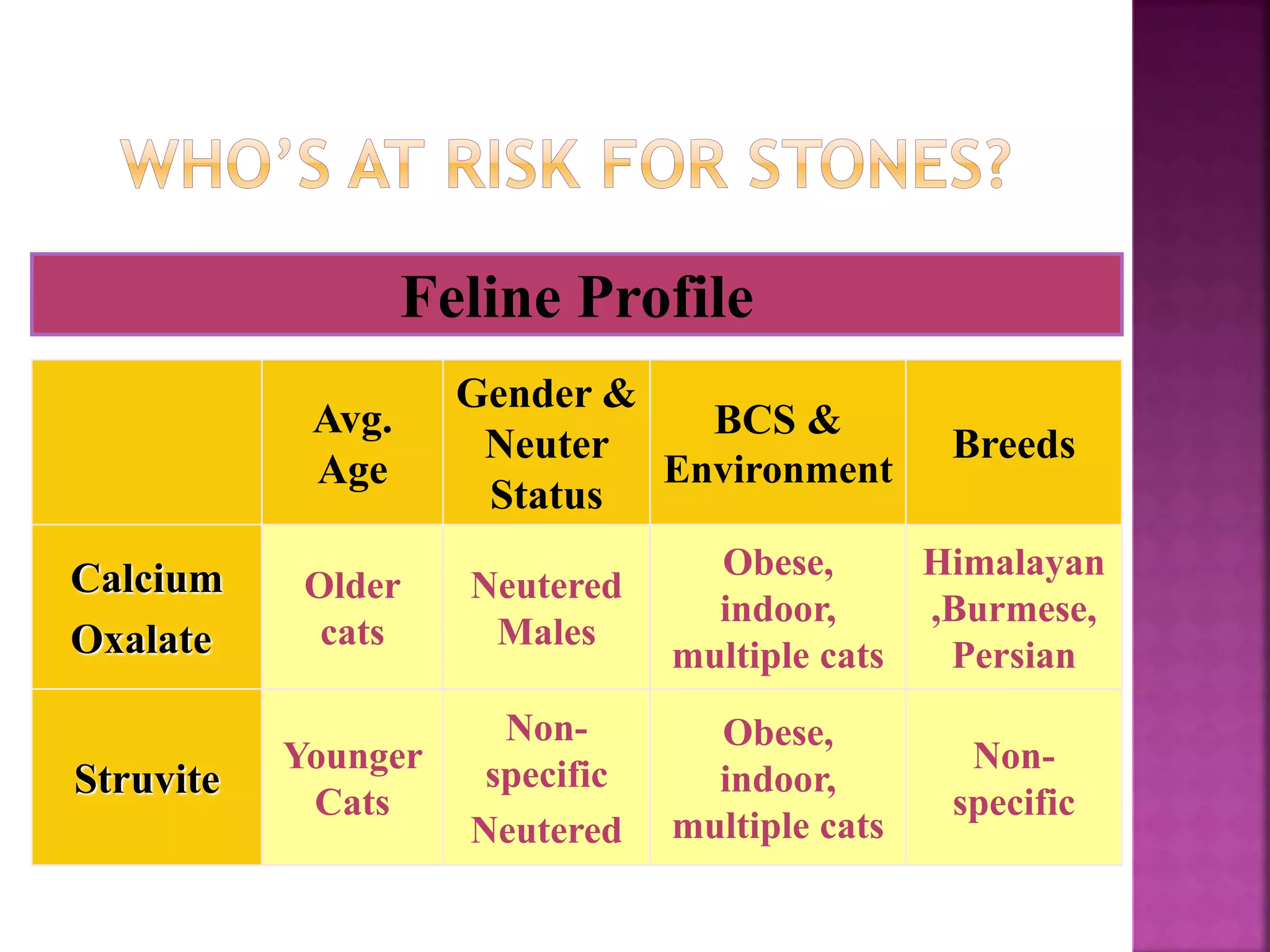
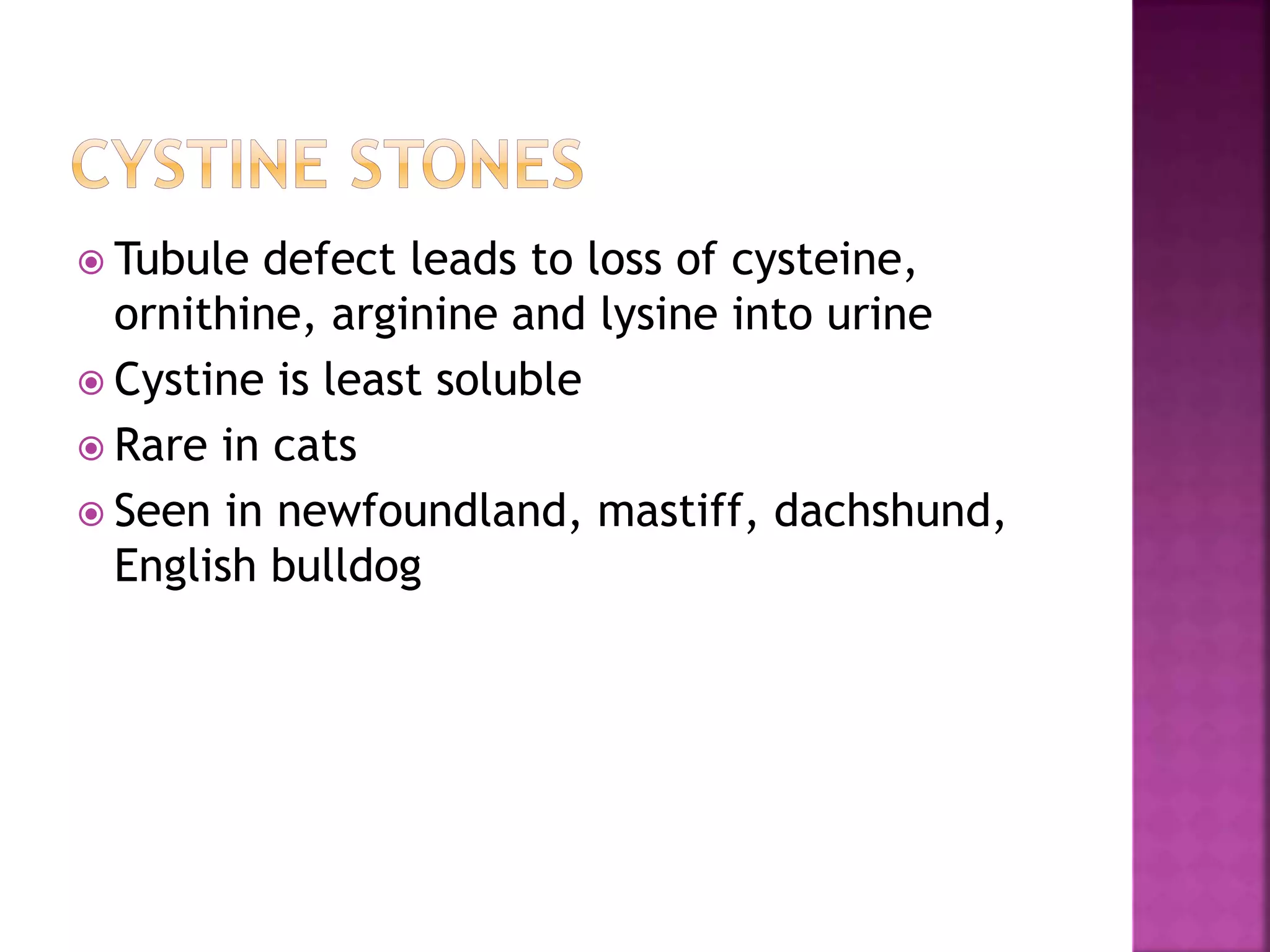
This document discusses various types of urinary tract diseases, gastrointestinal diseases, and liver diseases in pets and their nutritional management. For urinary tract diseases like struvite and calcium oxalate uroliths, dietary changes can help dissolve or prevent further stone formation by altering the pH and mineral content of urine. Gastrointestinal diseases like inflammatory bowel disease and constipation may require hydrolyzed protein or fiber-modified diets. Liver diseases like portosystemic shunts and hepatic lipidosis need low protein diets to prevent neurological signs. Nutritional support is critical for pets with liver disease and failure.