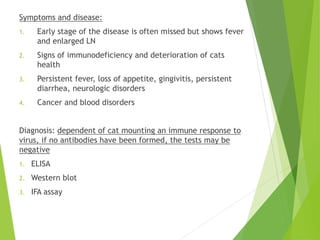
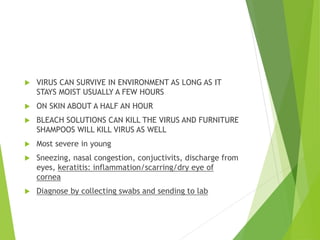
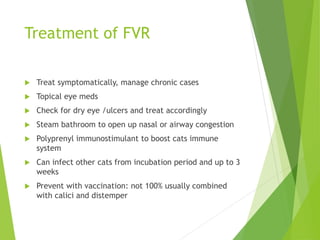
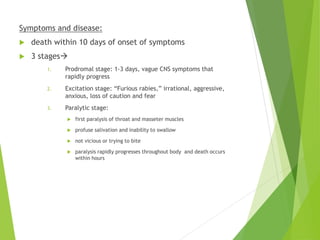
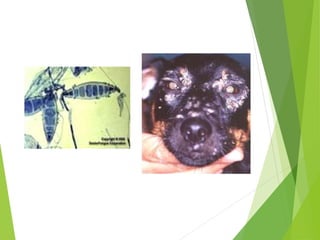
This document summarizes key information about viruses that commonly infect cats and dogs. It describes the structure and life cycle of viruses in general and then discusses several specific viral diseases including Feline Leukemia Virus (FeLV), Feline Immunodeficiency Virus (FIV), Feline Panleukopenia Virus (FPV), Feline Infectious Peritonitis (FIP), Feline Calicivirus (FCV), Feline Viral Rhinotracheitis, Rabies Virus, and Canine Distemper Virus. For each virus, it covers transmission, symptoms, diagnosis/testing, treatment/prevention strategies. Vaccination is emphasized as an important prevention method