The document discusses the importance of cytogenetic analysis in hematological malignancies. Some key points:
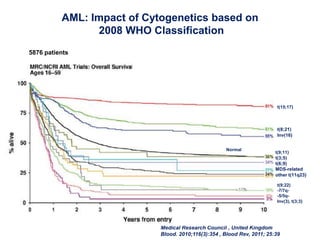
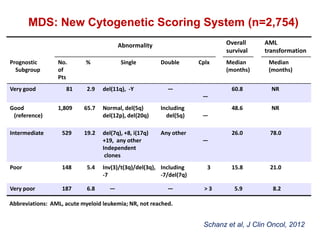
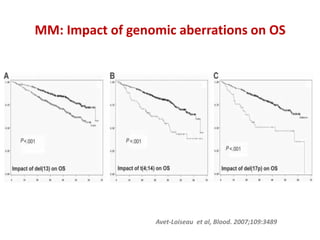
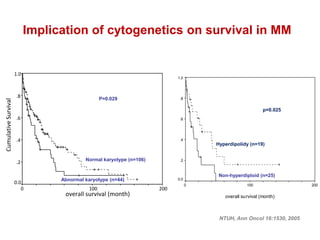
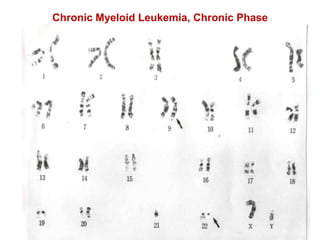
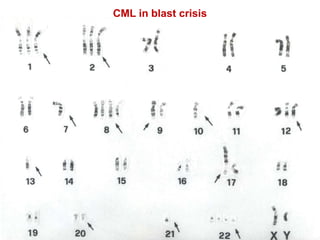
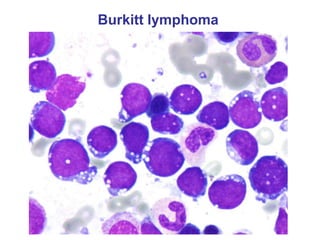
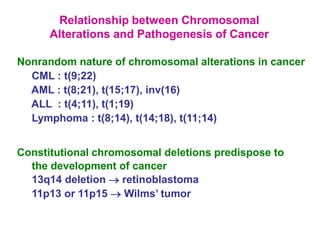
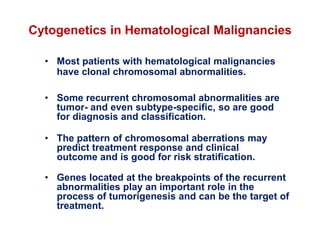
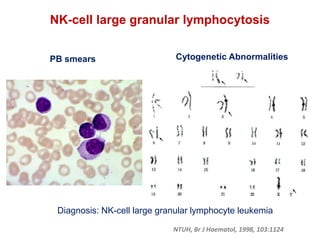
- Many hematological malignancies have clonal chromosomal abnormalities that can aid in diagnosis, classification, and risk stratification.
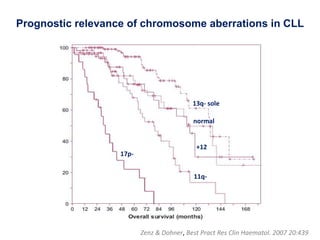
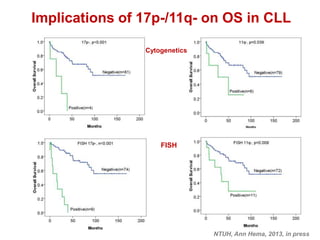
- Certain recurrent abnormalities are specific to certain tumor subtypes and can predict treatment response and clinical outcome.
- Genes at breakpoints of recurrent abnormalities play a role in tumorigenesis and can be treatment targets.
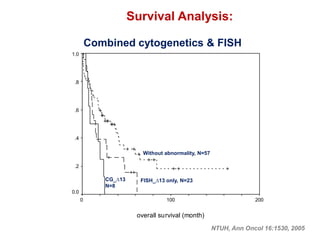
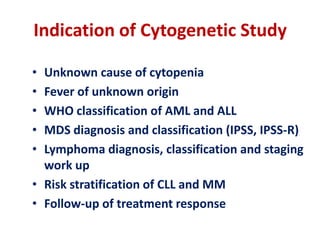
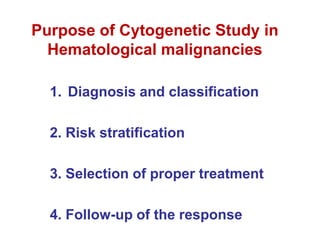
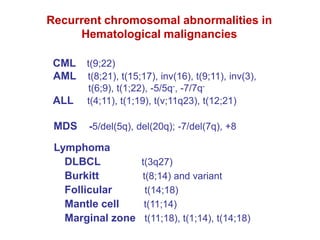
- Cytogenetic analysis is useful for diagnosis, risk stratification, treatment selection, and monitoring treatment response in hematological cancers like CML, AML, ALL, lymphoma, MDS, MM, and CLL.

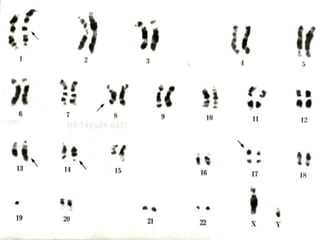
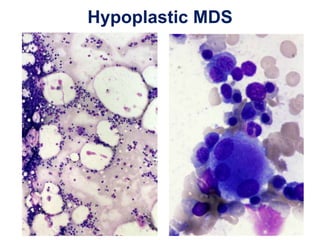
![Name: 林X榮,
46, XY, -7 [20]
Chromosomal abnormality
Diagnosis: hypoplastic MDS
NTUH, Leukemia, 2008, 22:544](https://image.slidesharecdn.com/03cytogeneticanalysisinhemamalgfinal-130823175312-phpapp02/85/Cytogenetic-Analysis-in-Hematological-Malignancies-11-320.jpg)