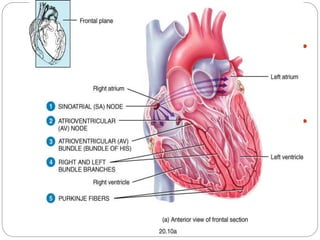
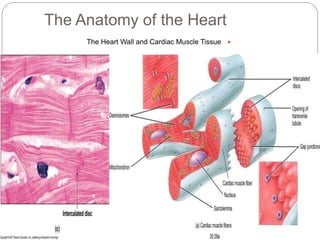
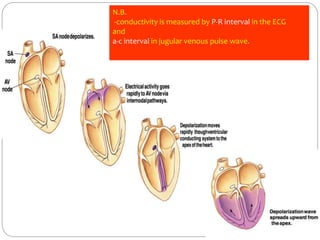
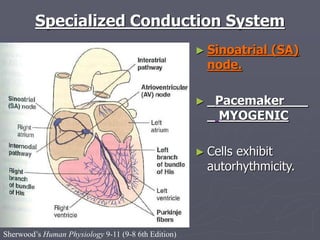
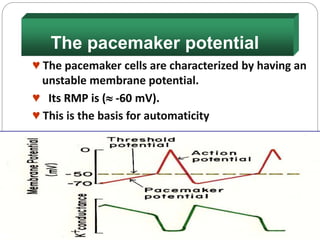
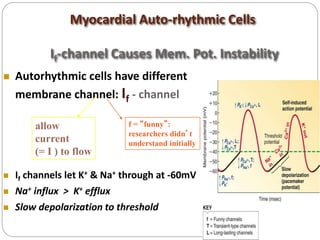
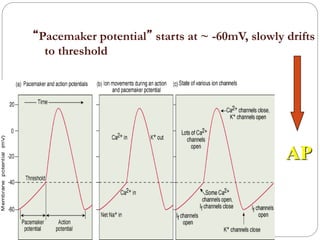
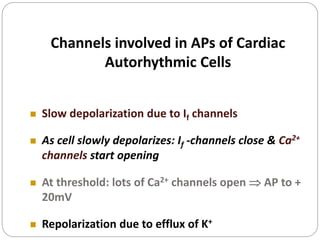
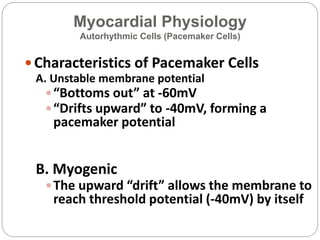
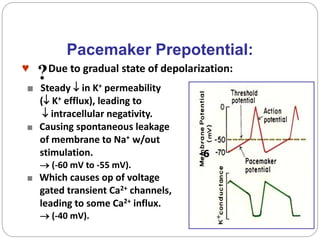
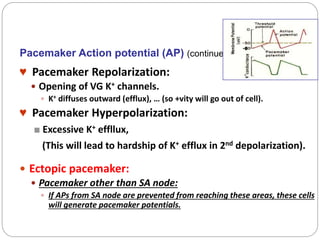
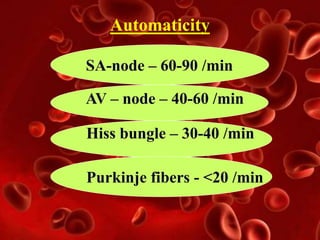
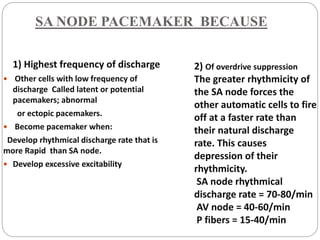
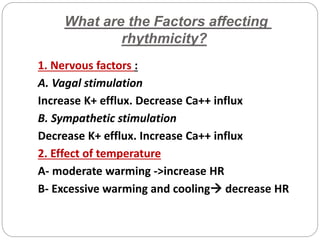
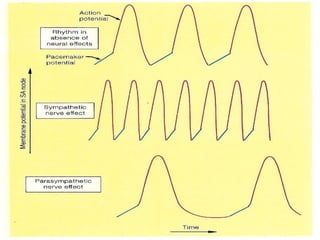
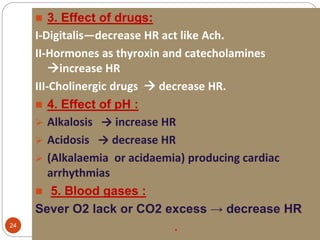
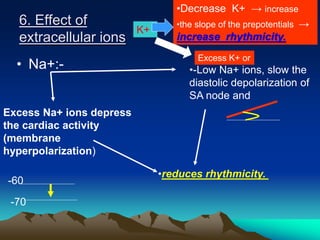
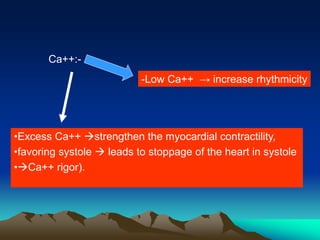
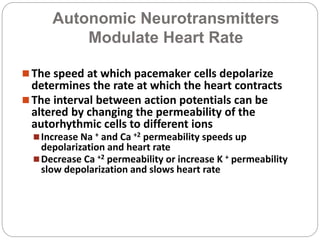
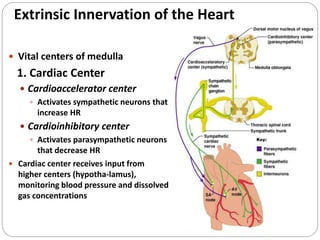
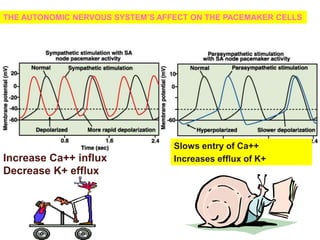
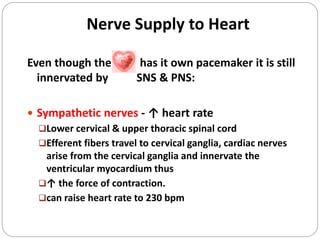
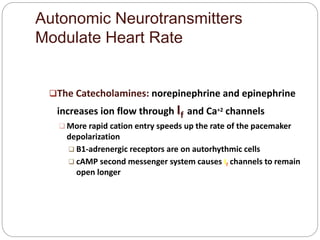
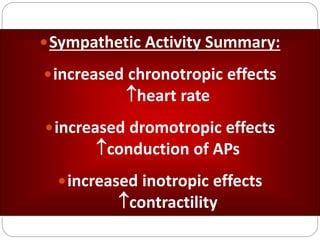
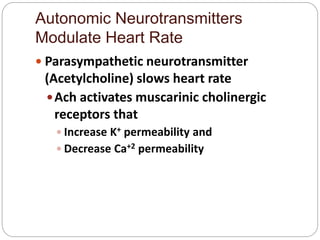
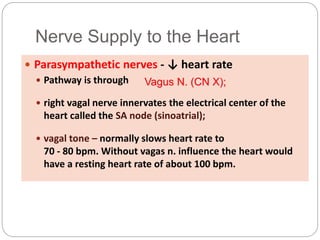
The document discusses the rhythmicity and pacemaker potential of the heart. It defines rhythmicity as the heart's ability to beat rhythmically due to action potentials it generates autonomously. The sinoatrial node is identified as the primary pacemaker of the heart due to its highest rate of discharge. Pacemaker cells in the sinoatrial node have an unstable membrane potential that allows them to slowly depolarize from -60mV to the threshold of -40mV, generating the pacemaker potential which initiates the cardiac action potential. Autonomic nerves also help regulate heart rate, with the sympathetic nervous system increasing rate and the parasympathetic nervous system decreasing it.