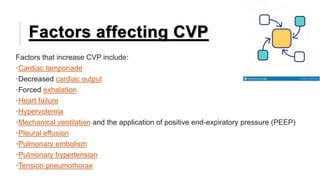
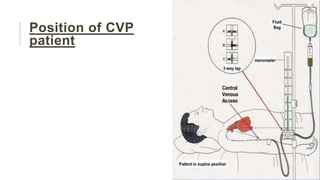
This document discusses central venous pressure (CVP), including how it is measured, normal ranges, factors that affect it, and implications of low or elevated CVP. CVP can be measured using a central venous catheter placed in the superior vena cava near the right atrium. It is affected by factors like volume status, heart function, and mechanical ventilation. Low CVP may indicate hypovolemia while elevated CVP can occur in heart failure. Measuring CVP provides information about a patient's fluid balance, circulating blood volume, and right heart function in critical care settings.
![VIVEKANANDA COLLEGE OF NURSING
MICRO-TEACHING PRACTICE
PRESENTED BY- APURVA DWIVEDI [M.Sc. NSG. 1ST YR.]](https://image.slidesharecdn.com/cvpmicroteaching-220717125721-cbc6a744/85/CVP-micro-teaching-pptx-1-320.jpg)


![Site
Normal
pressure range
(in mmHg)[5]
Central venous pressure 3–8
Right ventricular pressure
systolic 15–30
diastolic 3–8
Pulmonary artery pressure
systolic 15–30
diastolic 4–12
Pulmonary vein/
Pulmonary capillary wedge pressure
2–15
Left ventricular pressure
systolic 100–140
diastolic 3–12](https://image.slidesharecdn.com/cvpmicroteaching-220717125721-cbc6a744/85/CVP-micro-teaching-pptx-6-320.jpg)