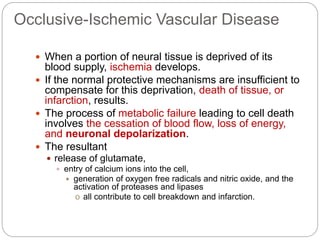
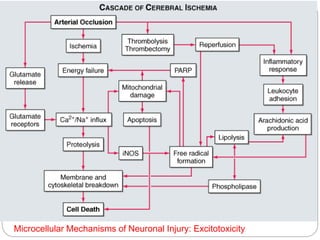
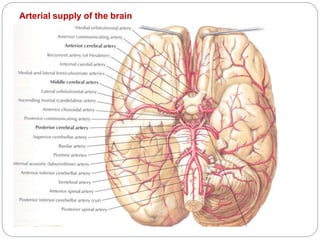
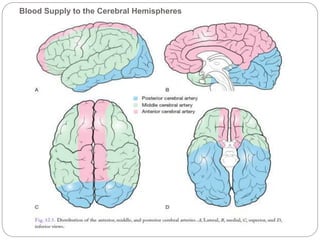
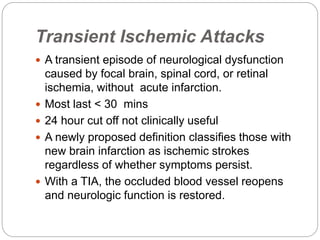
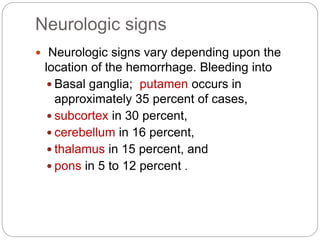
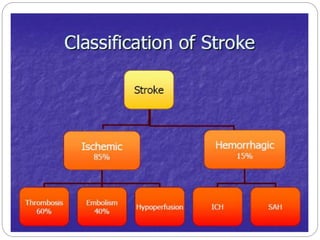
This document outlines a presentation on stroke. It begins with an introduction and classification of stroke, followed by sections on risk factors, pathophysiology, signs and symptoms, differential diagnosis, and approach to patients. It discusses that stroke is caused by a lack of blood flow to the brain and defines different types of stroke, including ischemic and hemorrhagic. Risk factors highlighted include age, hypertension, cardiac issues, and genetic factors. Signs and symptoms vary depending on the location and type of stroke.


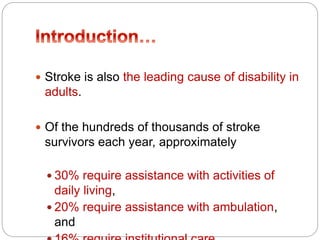
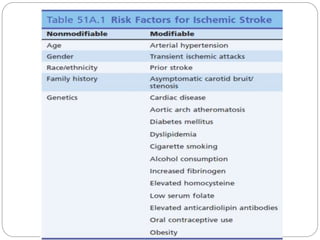


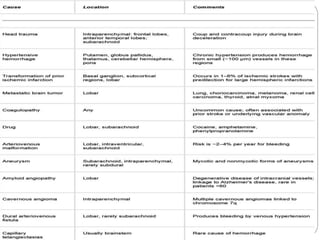
![Uncommon
Causes
Hypercoagulable disorders
Protein C deficiency
Protein S deficiency
Antithrombin III deficiency
Antiphospholipid syndrome
Factor V Leiden mutationa
Prothrombin G20210 mutationa
Systemic malignancy
Sickle cell anemia
Systemic lupus erythematosu
DIC
Nephrotic syndrome
Inflammatory bowel disease
Oral contraceptives
Venous sinus thrombosisb
Vasculitis
Systemic vasculitis [PAN,
granulomatosis with polyangiitis
(Wegener's), Takayasu's, & giant
cell arteritis]
Primary CNS vasculitis
Meningitis (syphilis, tuberculosis,
fungal, bacterial, zoster)
Cardiogenic
Mitral valve calcification
Atrial myxoma
Intracardiac tumor
Libman-Sacks endocarditis
Subarachnoid hemorrhage
vasospasm
Drugs: cocaine, amphetamin
Eclampsia](https://image.slidesharecdn.com/2-190511144646/85/2-stroke-10-320.jpg)