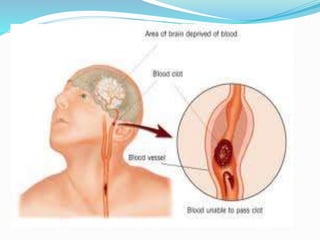
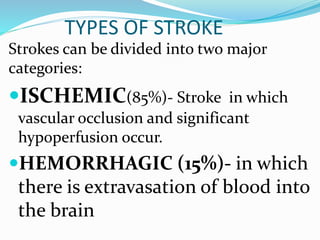
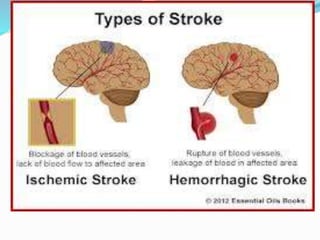
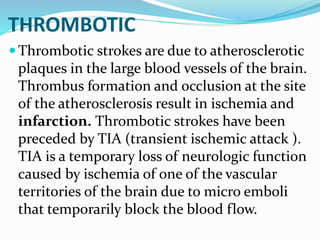
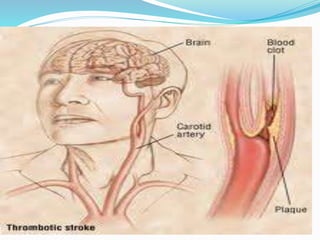
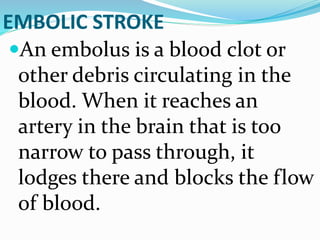
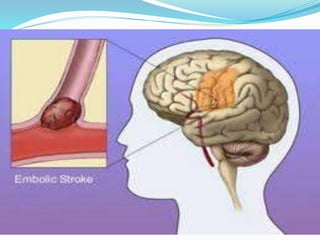
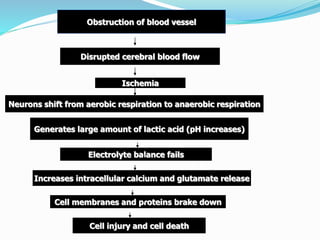
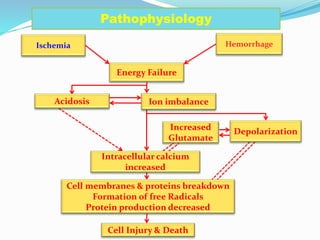
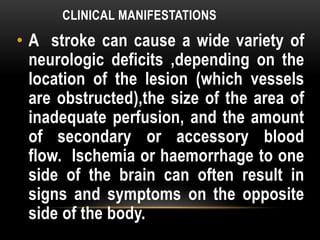
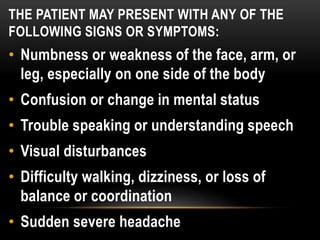
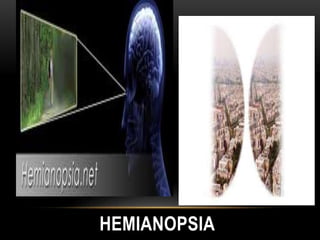
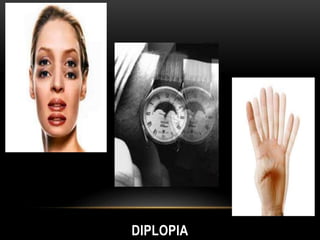
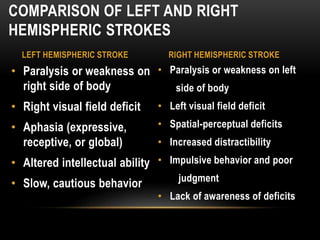
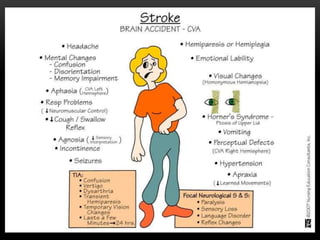
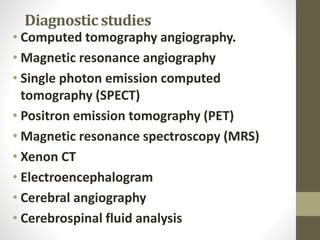
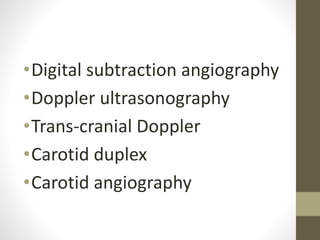
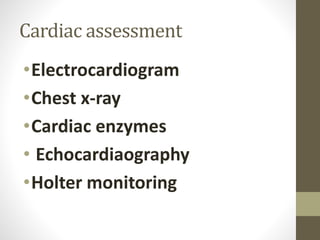
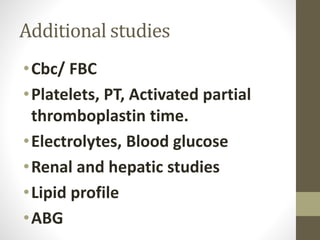
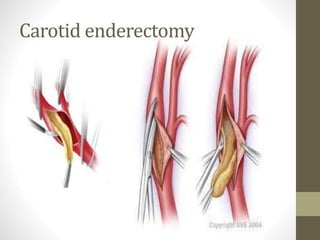
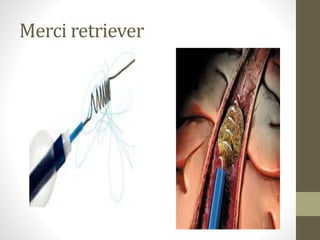
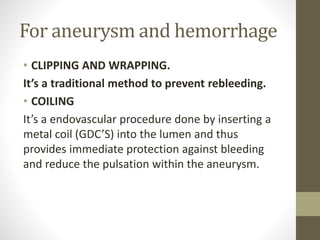
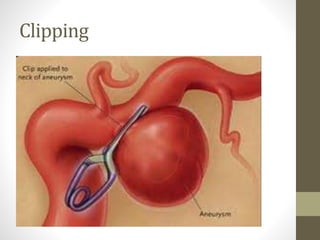
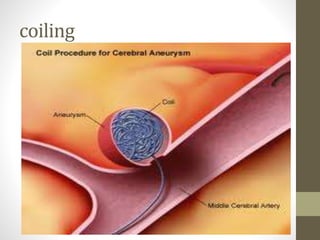
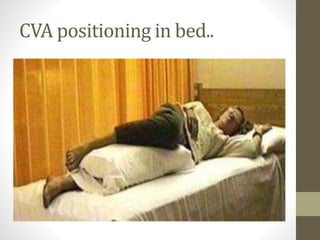
The document discusses stroke (also known as cerebrovascular accident or CVA), including its causes, types, risk factors, symptoms, diagnosis, and treatment. A stroke occurs when blood flow to the brain is interrupted, either by a blockage (ischemic stroke) or bleeding (hemorrhagic stroke). Diagnostic tests help determine the location and size of the affected area. Treatment involves both pharmacological measures such as antiplatelet drugs and surgery for high-risk conditions, as well as lifestyle modifications and rehabilitation. Nursing care focuses on improving mobility and preventing complications.