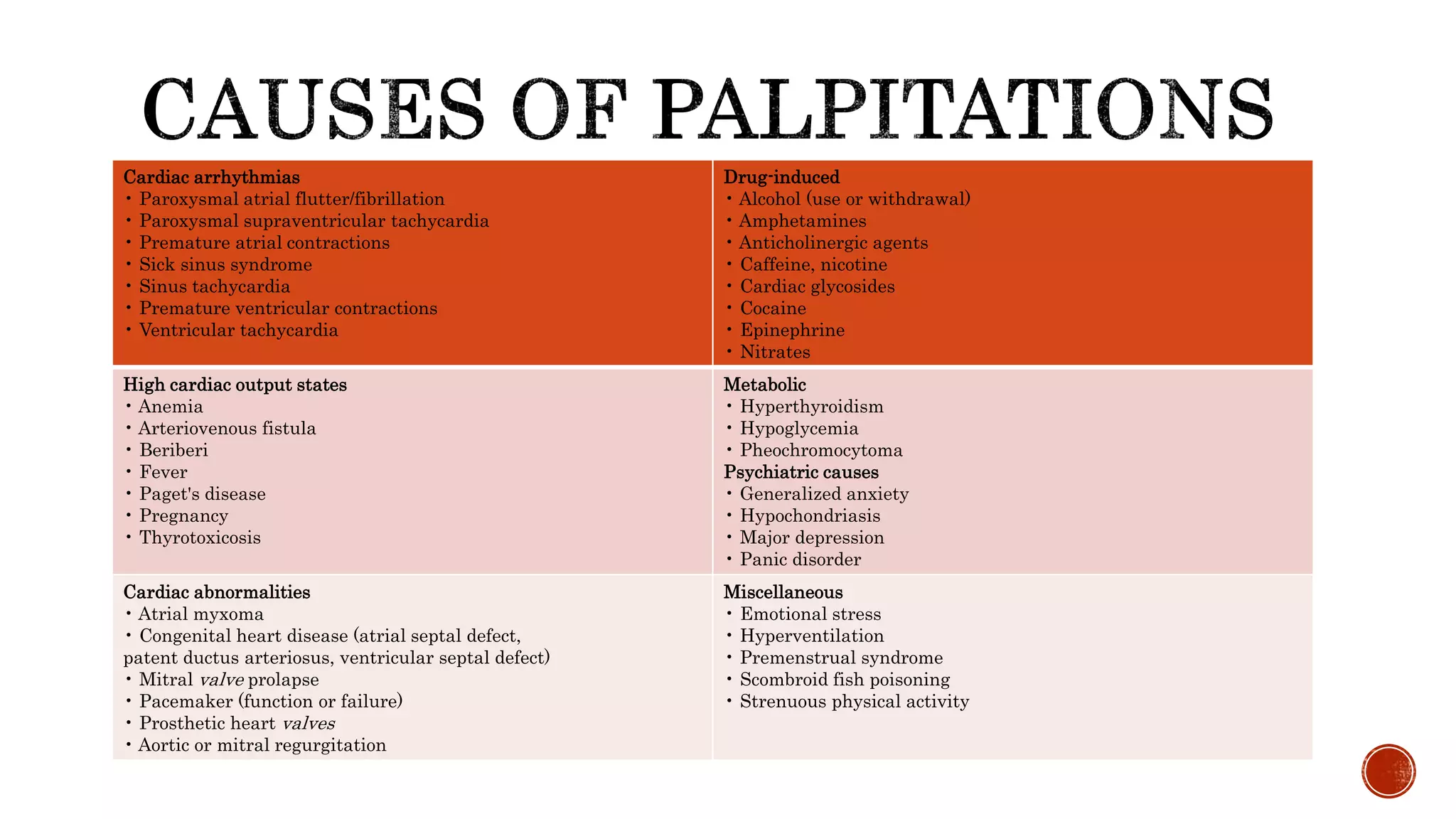
Palpitations refer to an uncomfortable awareness of one's own heartbeat and can occur due to cardiac arrhythmias, drug or substance use, medical conditions affecting the heart or metabolism, psychiatric issues, or structural heart abnormalities. A thorough history and physical exam aims to determine the nature, triggers, and underlying cause of the palpitations. Additional testing like ECG, Holter monitoring, echocardiogram, or electrophysiology study may help detect and diagnose any cardiac arrhythmias present.