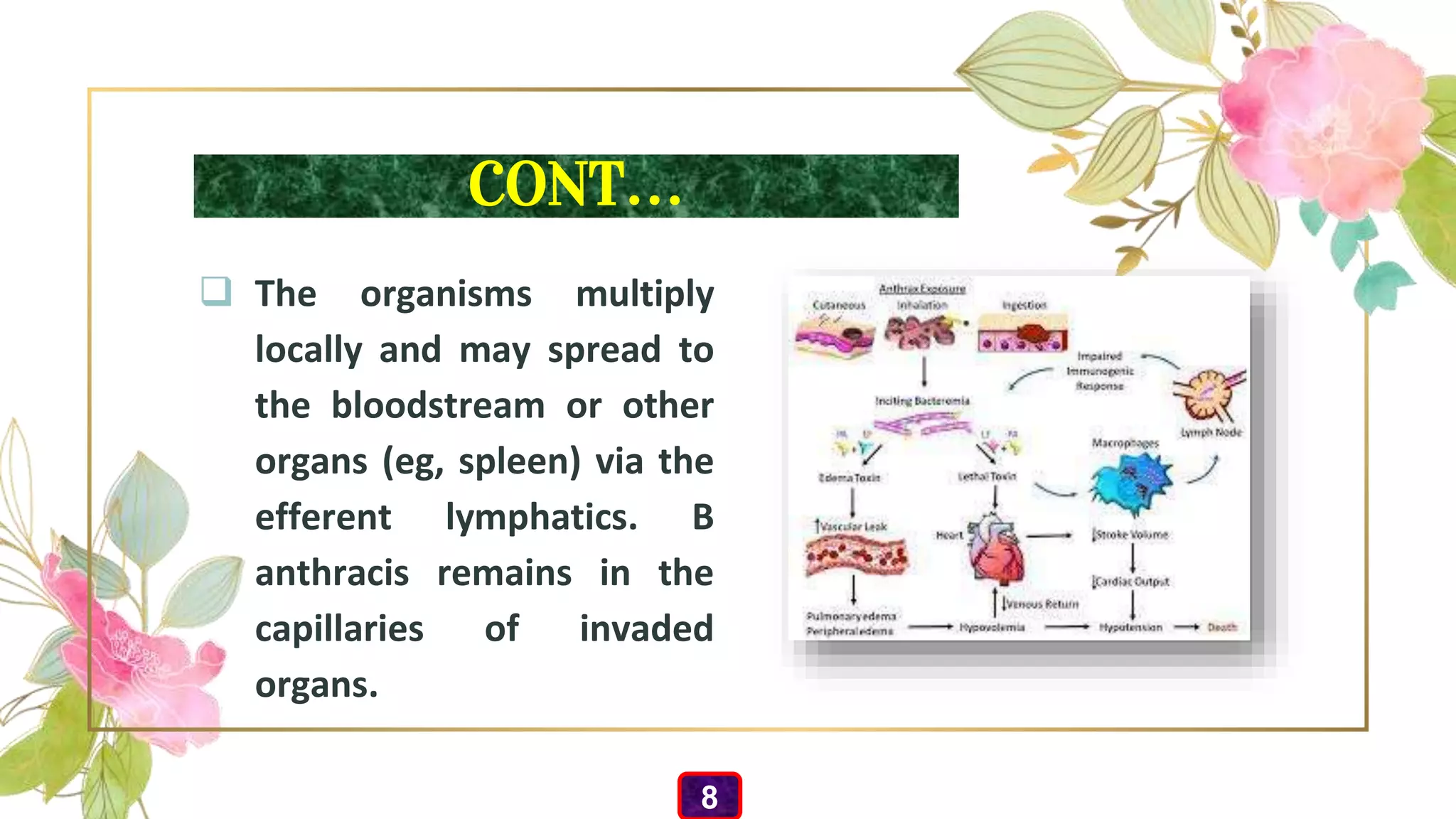
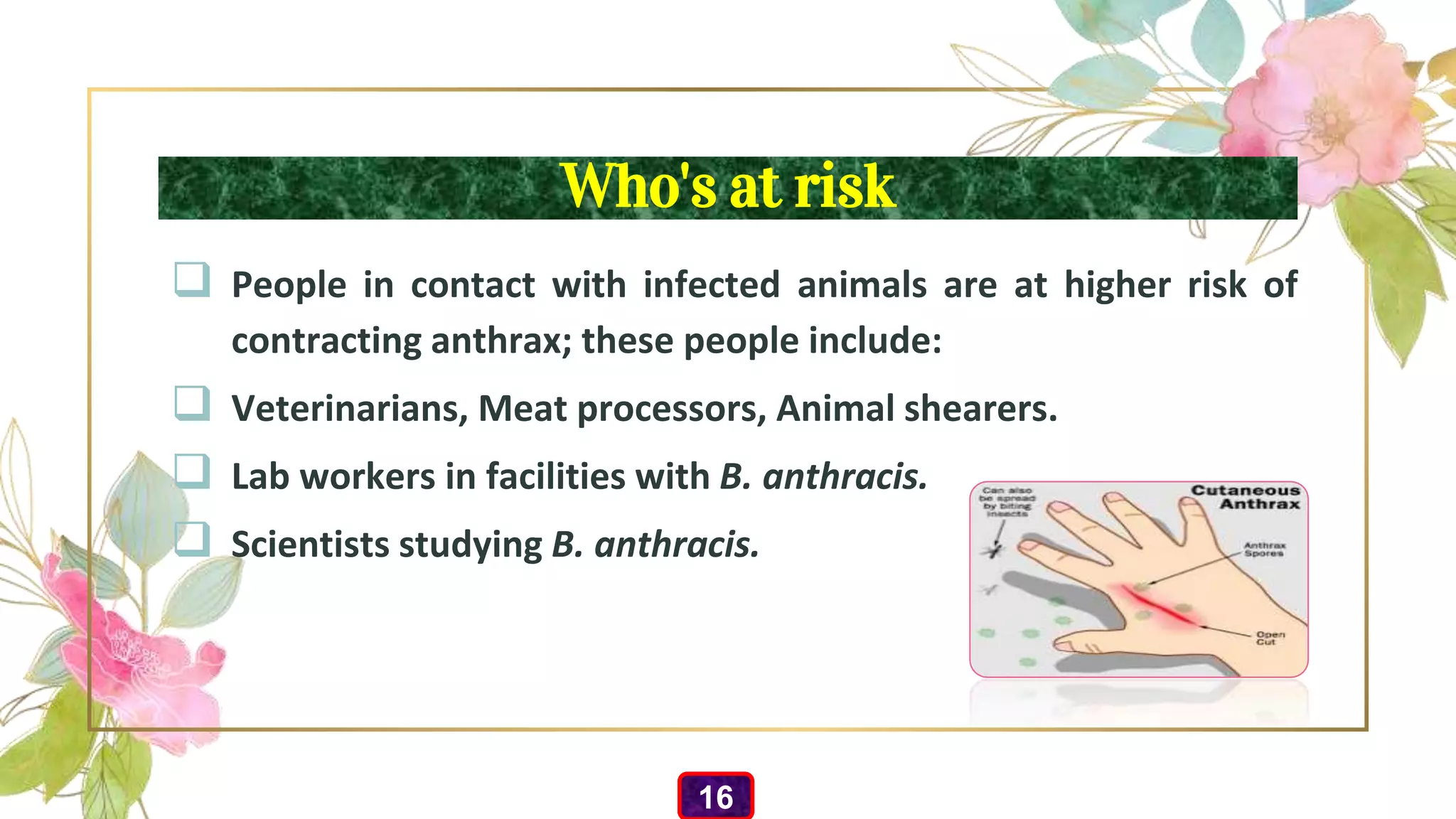
Cutaneous anthrax is the most common and least dangerous form of anthrax infection, caused by the bacterium Bacillus anthracis, which typically enters through breaks in the skin. Transmission occurs primarily through handling contaminated animal products, and symptoms include blisters, swelling, and a painless ulcer with a black center. The document discusses historical context, epidemiology, diagnosis, prevention, treatments, and risk factors associated with cutaneous anthrax.