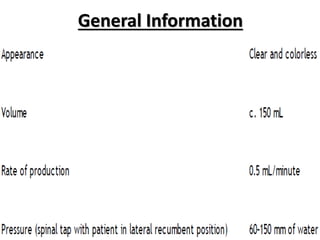
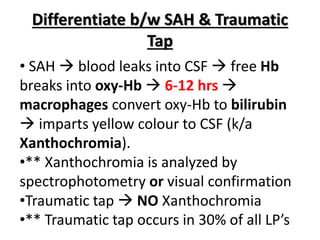
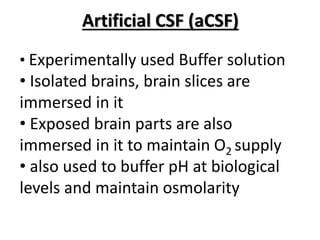
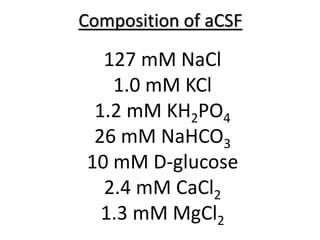
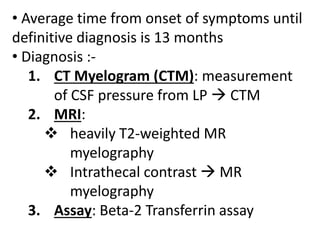
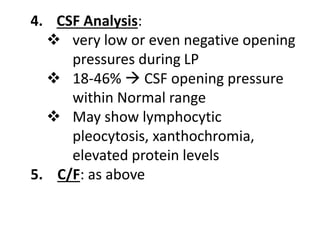
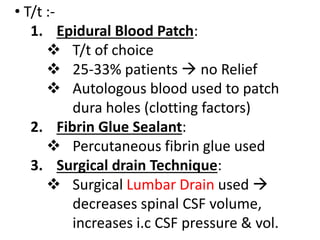
The document discusses the formation and analysis of cerebrospinal fluid (CSF), detailing the differences between subarachnoid hemorrhage (SAH) and traumatic taps in lumbar punctures. It covers the characteristics and treatment options for spontaneous intracranial hypotension (SIH), which is a condition resulting from CSF leaks causing severe headaches and other symptoms. It concludes with treatment methods such as epidural blood patches and the challenges in achieving a definitive diagnosis.