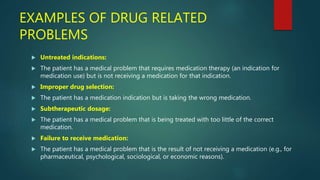
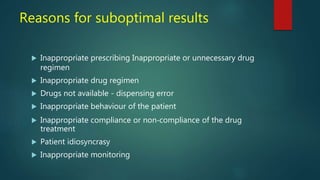
This document summarizes the concept of pharmaceutical care as presented by Shaista Sumayya, a 4th year PharmD student. It defines pharmaceutical care as the direct provision of medication-related care to improve patient outcomes. The pharmacist's role involves identifying and resolving drug-related problems by designing treatment plans, monitoring outcomes, and preventing potential issues. Key aspects of pharmaceutical care include collecting patient data, evaluating treatment alternatives, individualizing drug regimens, and documenting provided care. The overall goal is to cure diseases, reduce symptoms, and improve a patient's quality of life through optimized medication management.