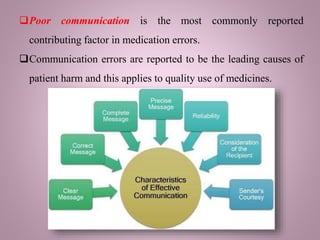
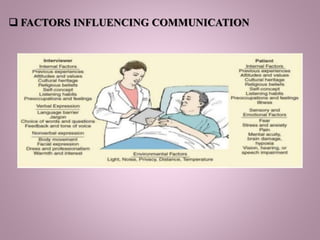
The document discusses the importance of effective communication for achieving quality use of medicines. It notes that clear communication is needed between doctors and patients to explain why medicines are prescribed, address any barriers to understanding, and identify all medications patients are taking. Poor communication has been shown to be a leading cause of medication errors and patient harm. The document emphasizes the role of communication skills like briefings, handovers, patient education materials, and electronic prescribing in improving safety. Overall, it stresses that open communication between healthcare providers and patients is critical to negotiate treatment outcomes, minimize risks, and promote appropriate medication use.