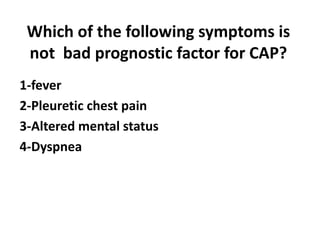
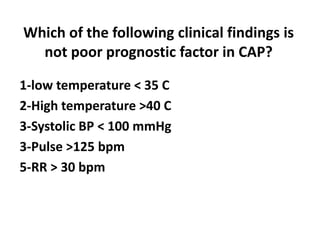
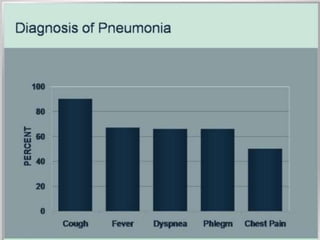
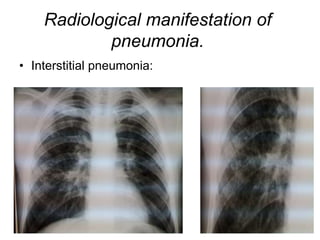
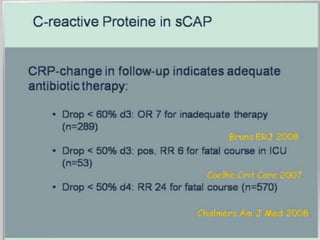
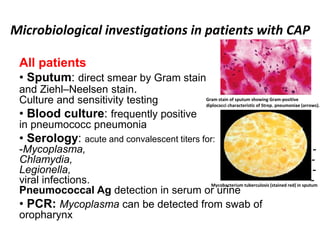
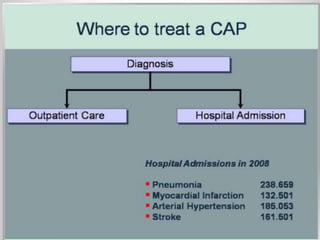
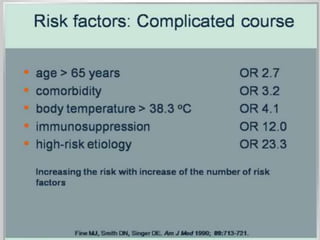
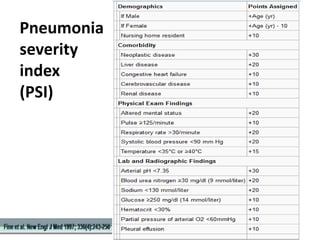
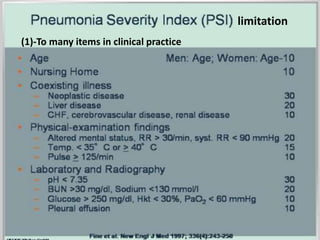
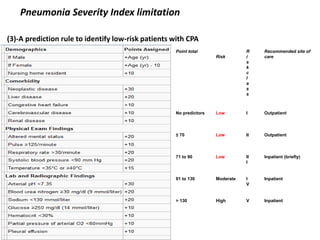
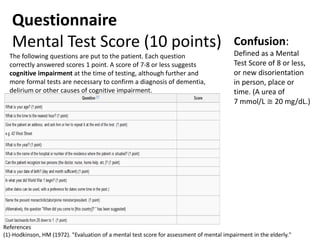
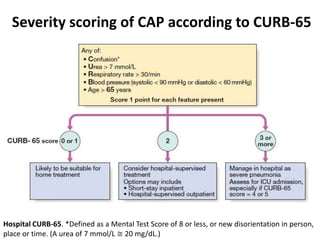
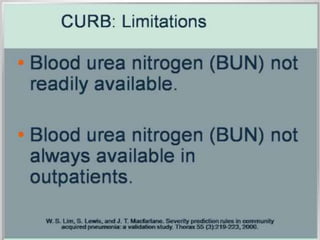
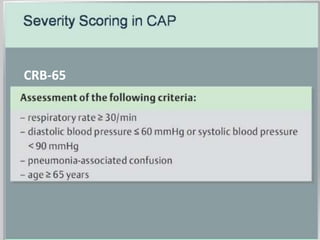
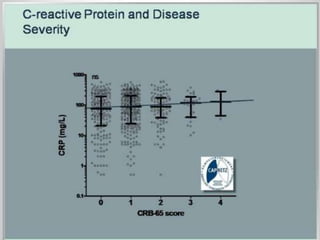
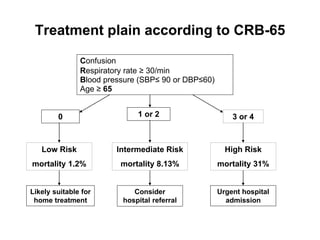
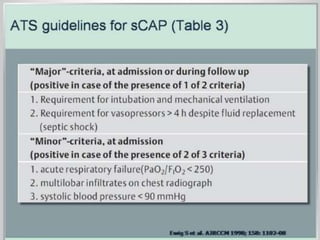
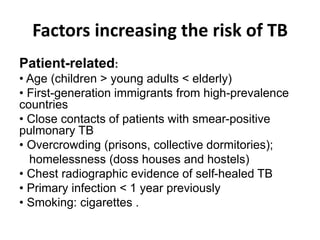
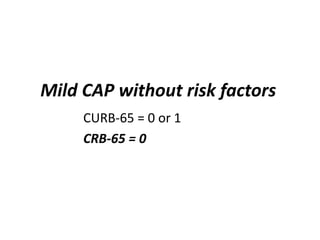
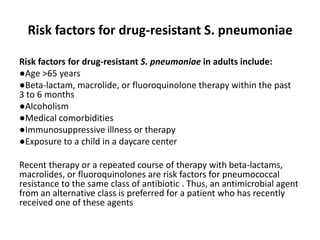
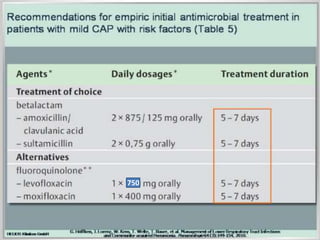
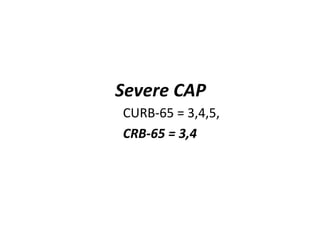
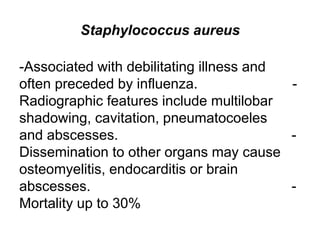
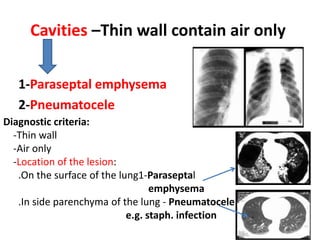
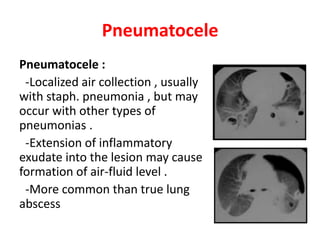
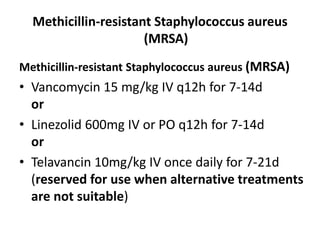
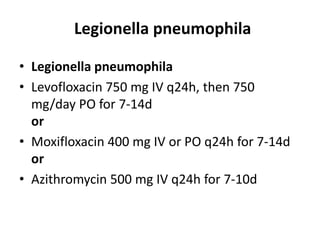
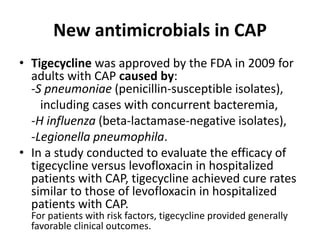
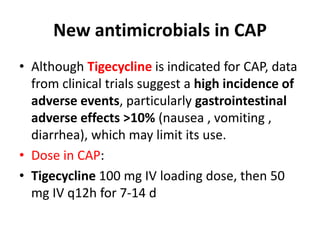
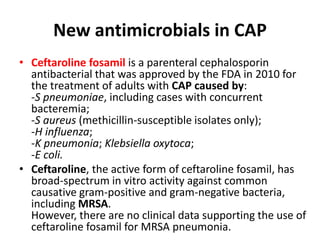
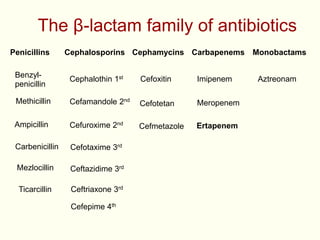
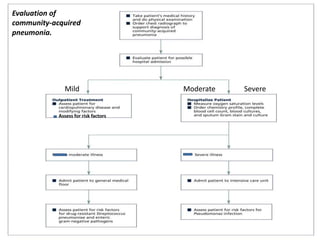
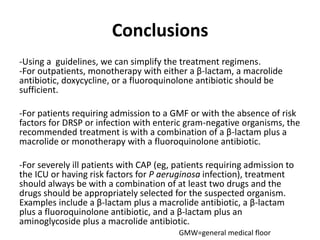
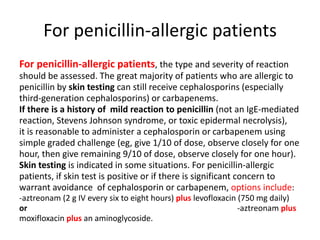
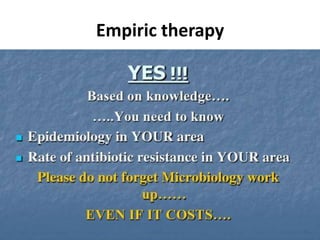
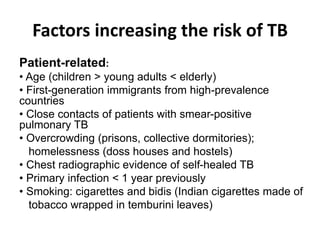
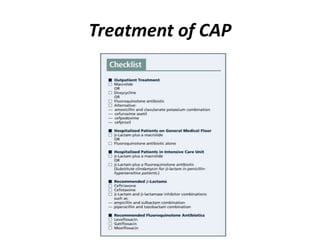
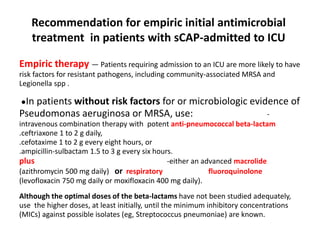
This document discusses community acquired pneumonia (CAP). It begins by defining CAP and discussing its epidemiology and classification. It then covers the incidence, clinical presentation, radiological manifestations, and typical microbiological findings of CAP. It discusses specific investigations and pathogens involved in severe CAP. Scoring systems for assessing CAP severity, including PSI, CURB-65 and CRB-65, are outlined. Guidelines are provided on treatment based on severity, including empiric antibiotic choice. Risk factors for drug-resistant pathogens and tuberculosis are noted. The document concludes with recommendations for empiric treatment of severe CAP patients admitted to the ICU.