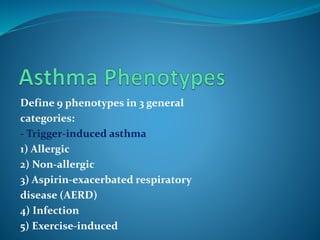
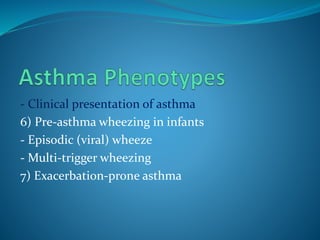
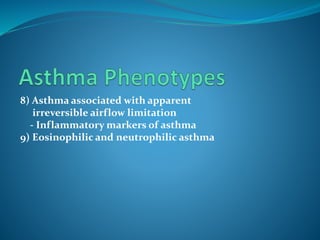
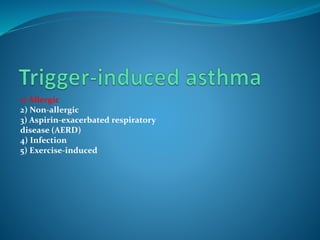
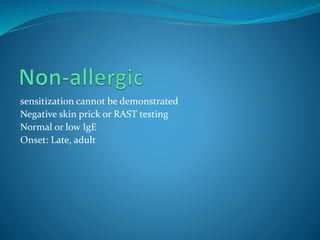
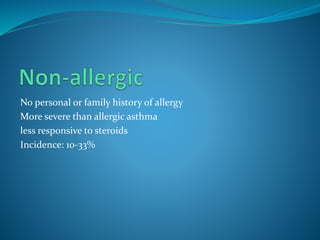
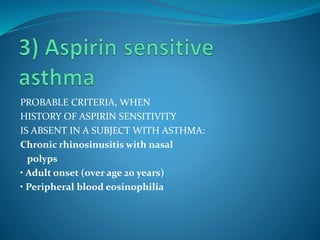
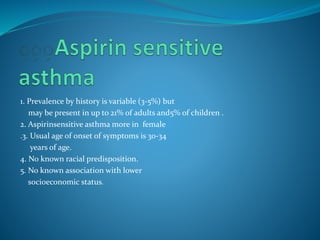
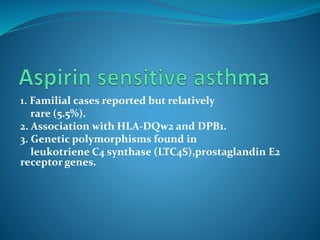
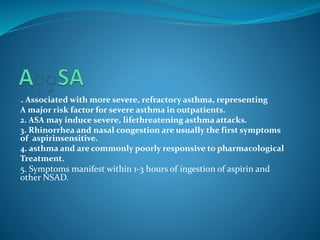
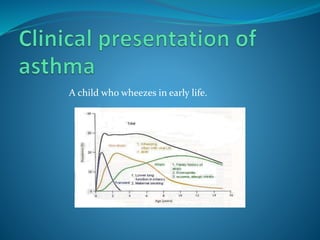
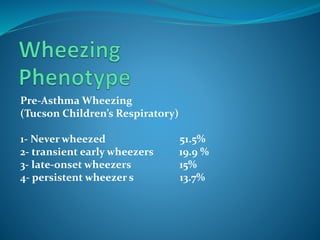
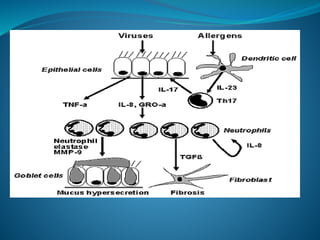
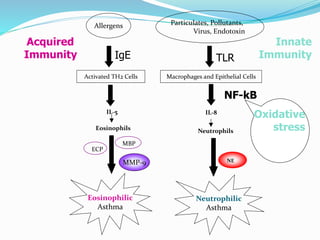
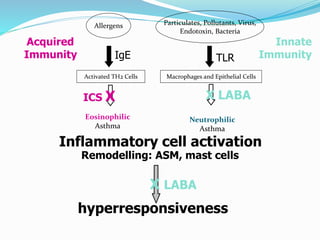
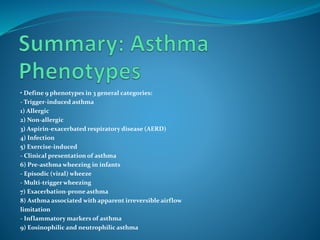
This document discusses expanding understanding of asthma phenotypes. It defines 9 asthma phenotypes in 3 categories: trigger-induced (allergic, non-allergic, aspirin-exacerbated respiratory disease, infection, exercise-induced), clinical presentation (pre-asthma wheezing in infants, exacerbation-prone), and inflammatory markers (eosinophilic and neutrophilic). Specific phenotypes like allergic asthma are more common in children while non-allergic asthma is more severe. Defining phenotypes enhances research by allowing appropriate study comparisons and correlating phenotypes with genotypes.