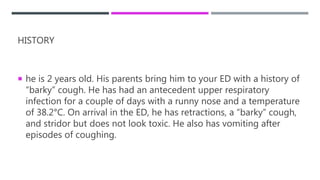
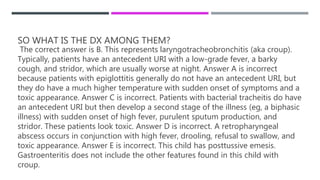
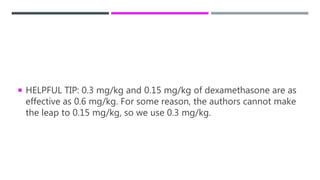
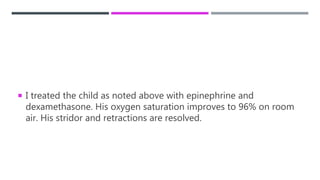
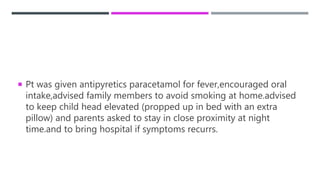
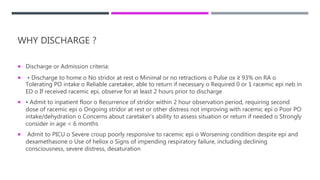
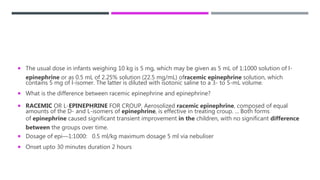
A 2-year-old boy presented to the emergency department with a barky cough, retractions, and stridor after a couple days of upper respiratory infection and fever. On examination he had retractions, barky cough, and stridor but did not appear toxic. The most likely diagnosis was laryngotracheobronchitis (croup). He was treated with nebulized racemic epinephrine, which resolved his stridor, and oral dexamethasone. After 2 hours of observation with improved symptoms, he was discharged home with instructions to return if symptoms recurred and advice on fever management and sleep positioning.