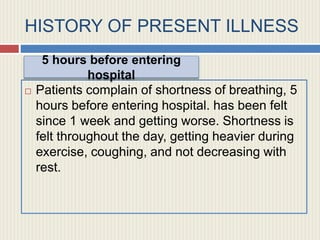
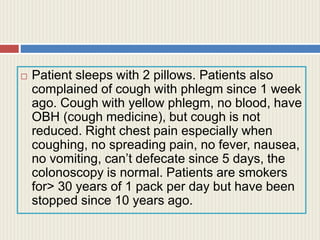
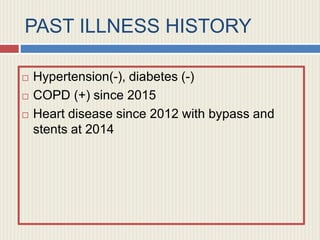
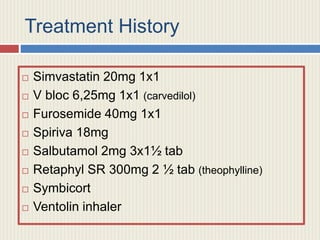
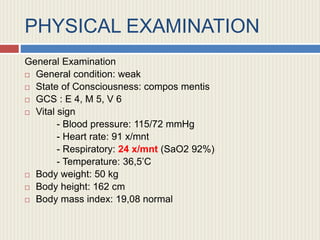
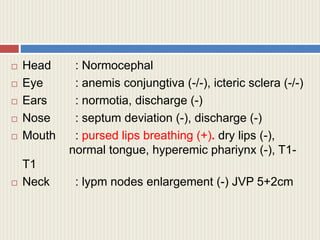
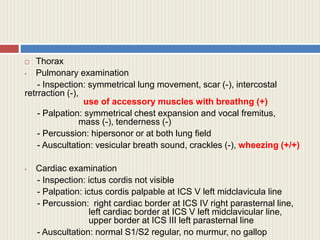
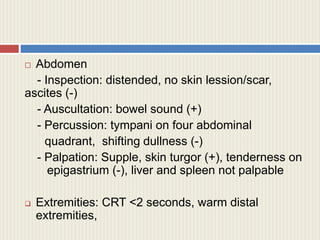
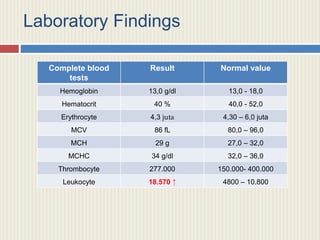
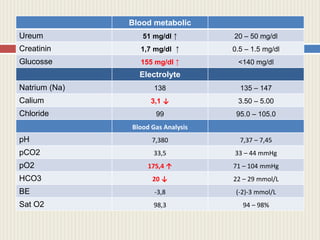
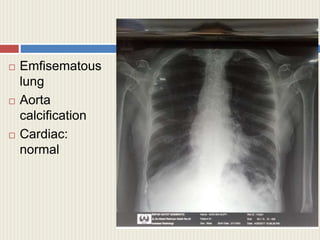
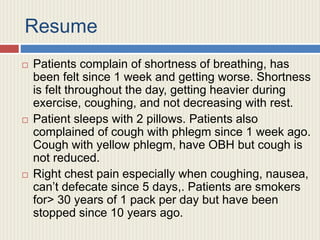
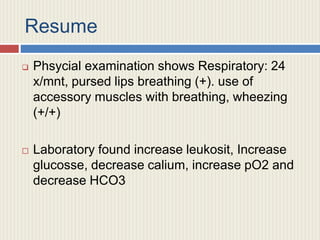
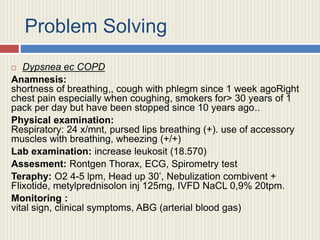
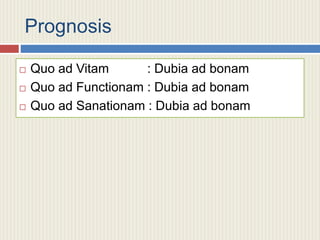
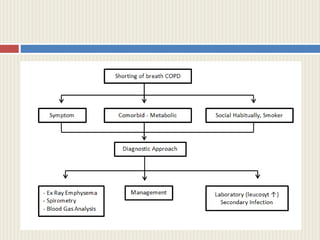
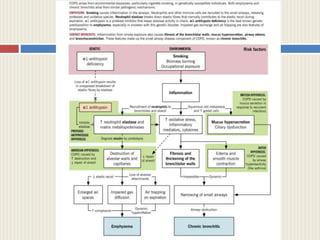
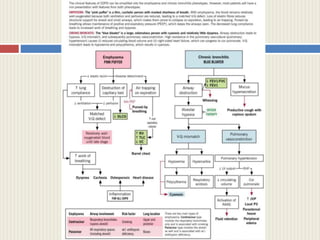
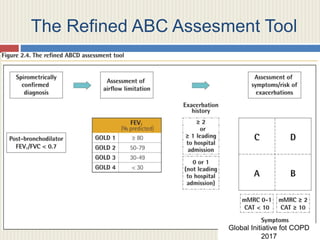
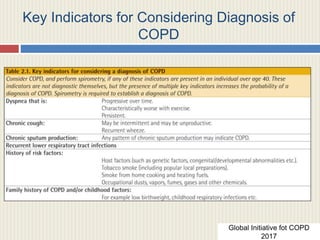
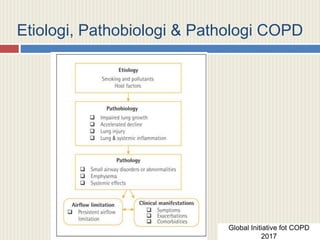
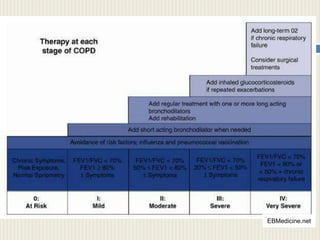
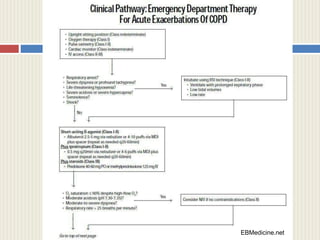
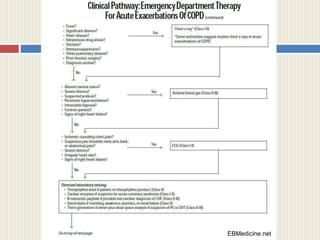
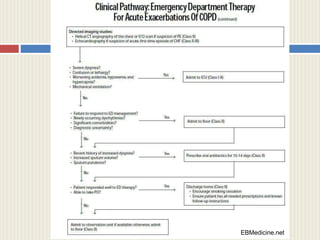
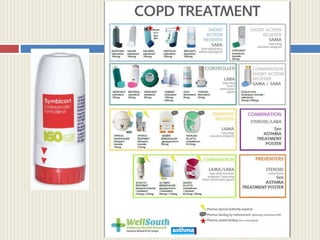
The document details a medical case of a 74-year-old male patient experiencing worsening shortness of breath and cough, diagnosed with Chronic Obstructive Pulmonary Disease (COPD). It includes patient history, physical examination findings, laboratory results, and treatment protocol. Key indicators for diagnosing COPD are also referenced, alongside prognosis and recommendations for management.