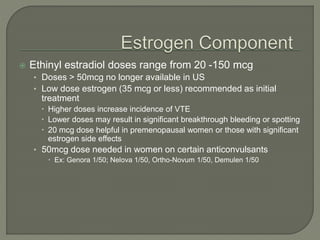
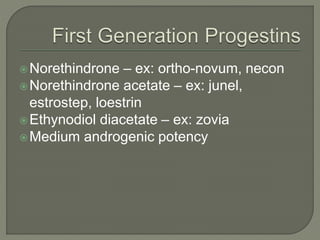
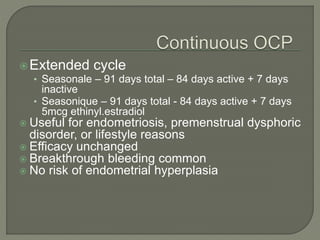
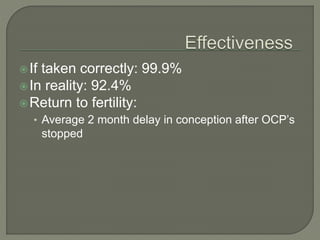
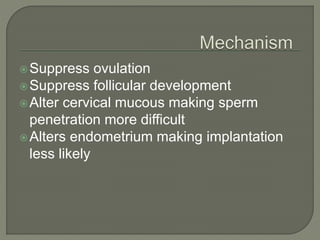
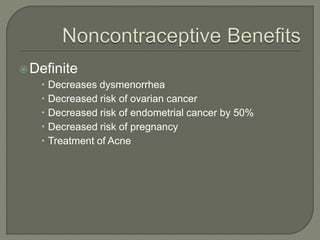
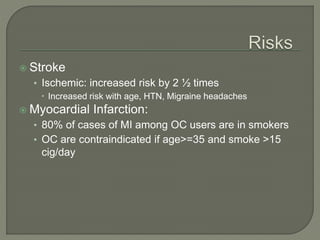
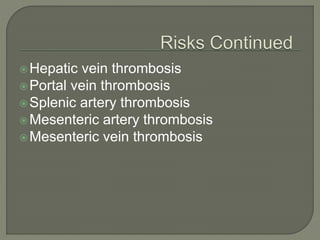
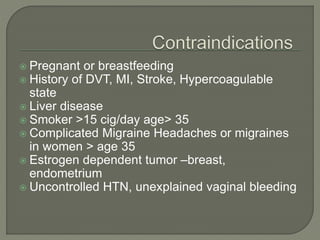
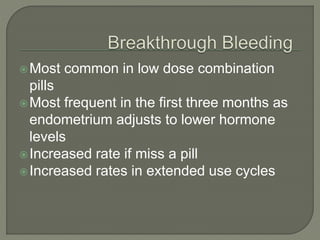
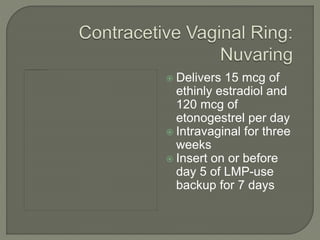
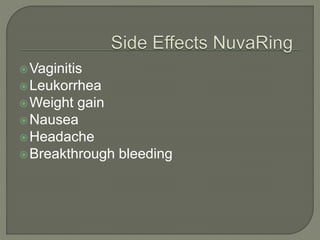
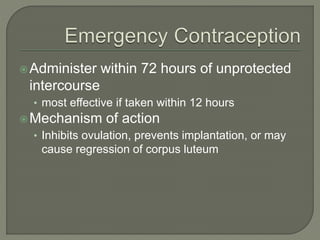
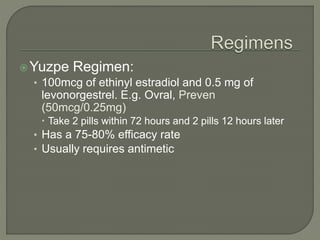
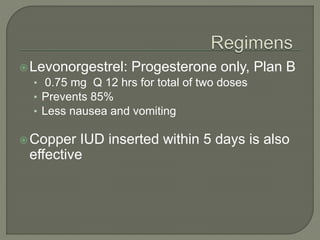
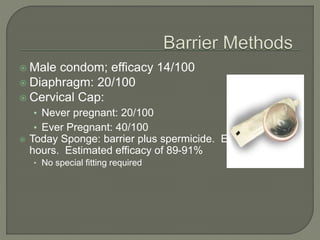
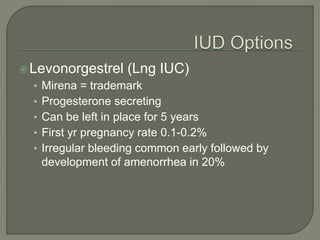
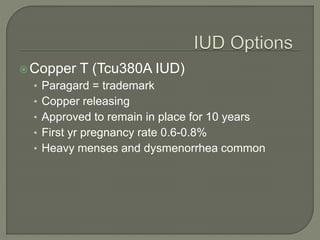
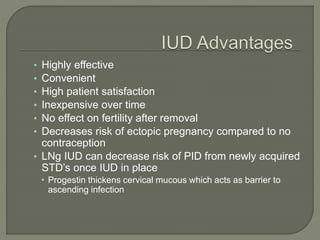
This document discusses various methods of contraception, including hormonal methods like oral contraceptives, barrier methods, intrauterine devices, and surgical methods like tubal ligation and vasectomy. It provides details on the mechanisms of action, effectiveness, advantages, and disadvantages of different contraceptive options to help health care providers choose appropriate contraception based on individual clinical situations.