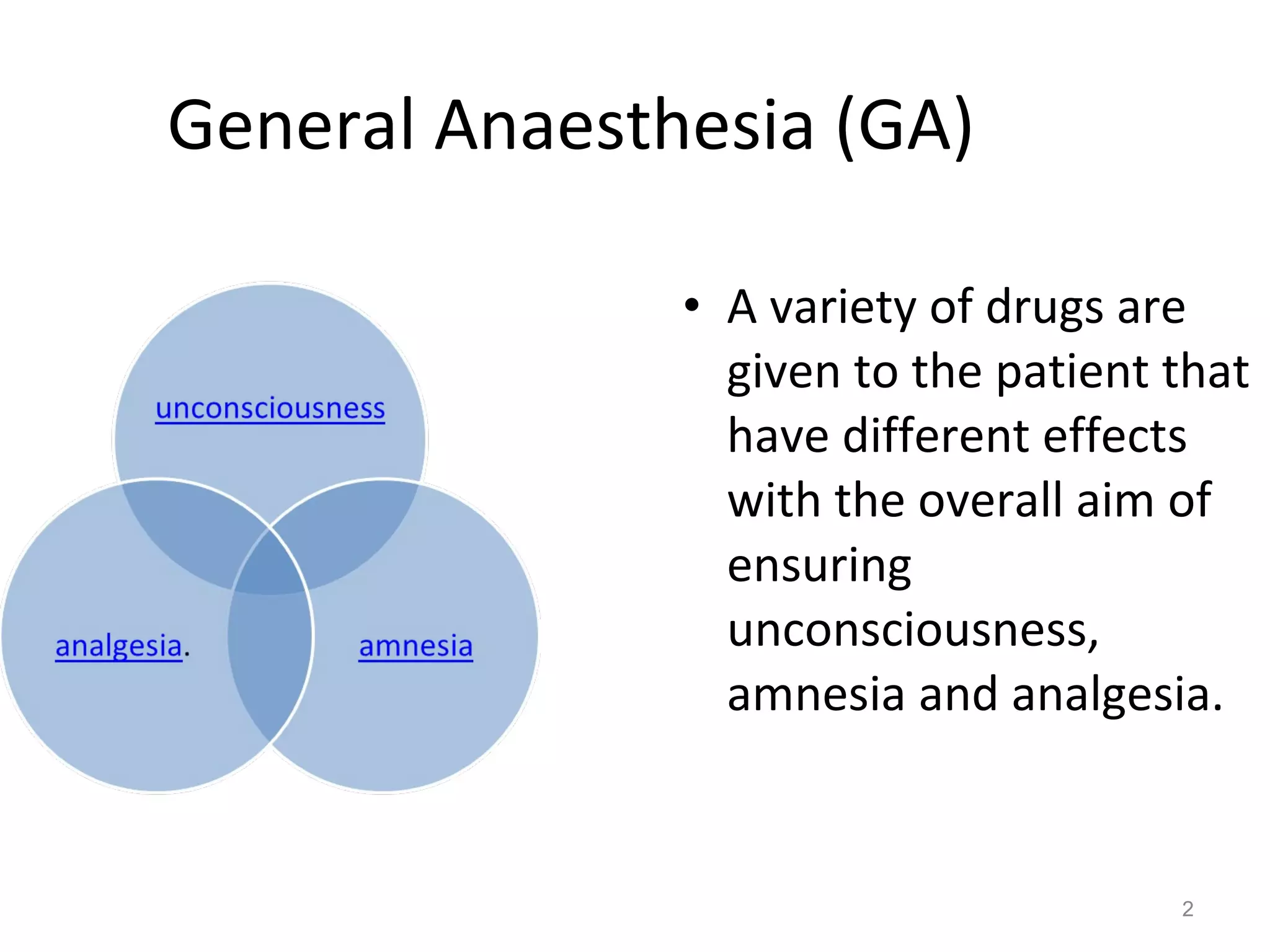
This document provides an overview of general anaesthesia, including:
- It involves pre-anaesthetic assessment, administration of anaesthetic drugs, cardio-respiratory monitoring, analgesia, airway management, and fluid management.
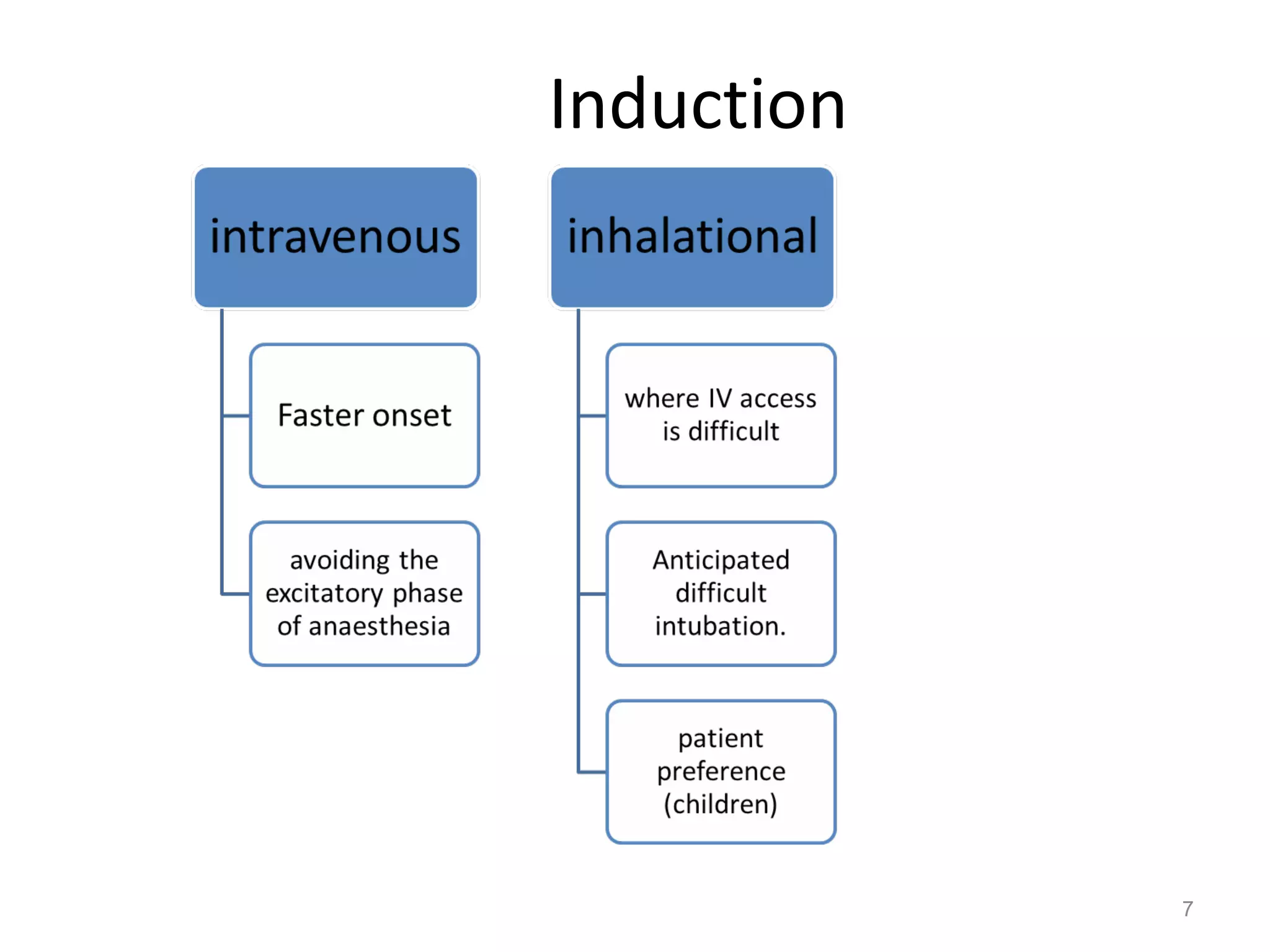
- Common intravenous induction agents are propofol, sodium thiopental, and ketamine which modulate GABA transmission.
- Inhalational induction options include sevoflurane which causes less irritation.
- Maintenance involves inhalation of oxygen, nitrous oxide, and volatile anaesthetic along with intravenous opioids. Total intravenous anaesthesia uses propofol infusion.
- Airway management often uses endotracheal tubes or laryngeal masks. Monitoring includes ECG, pulse ox