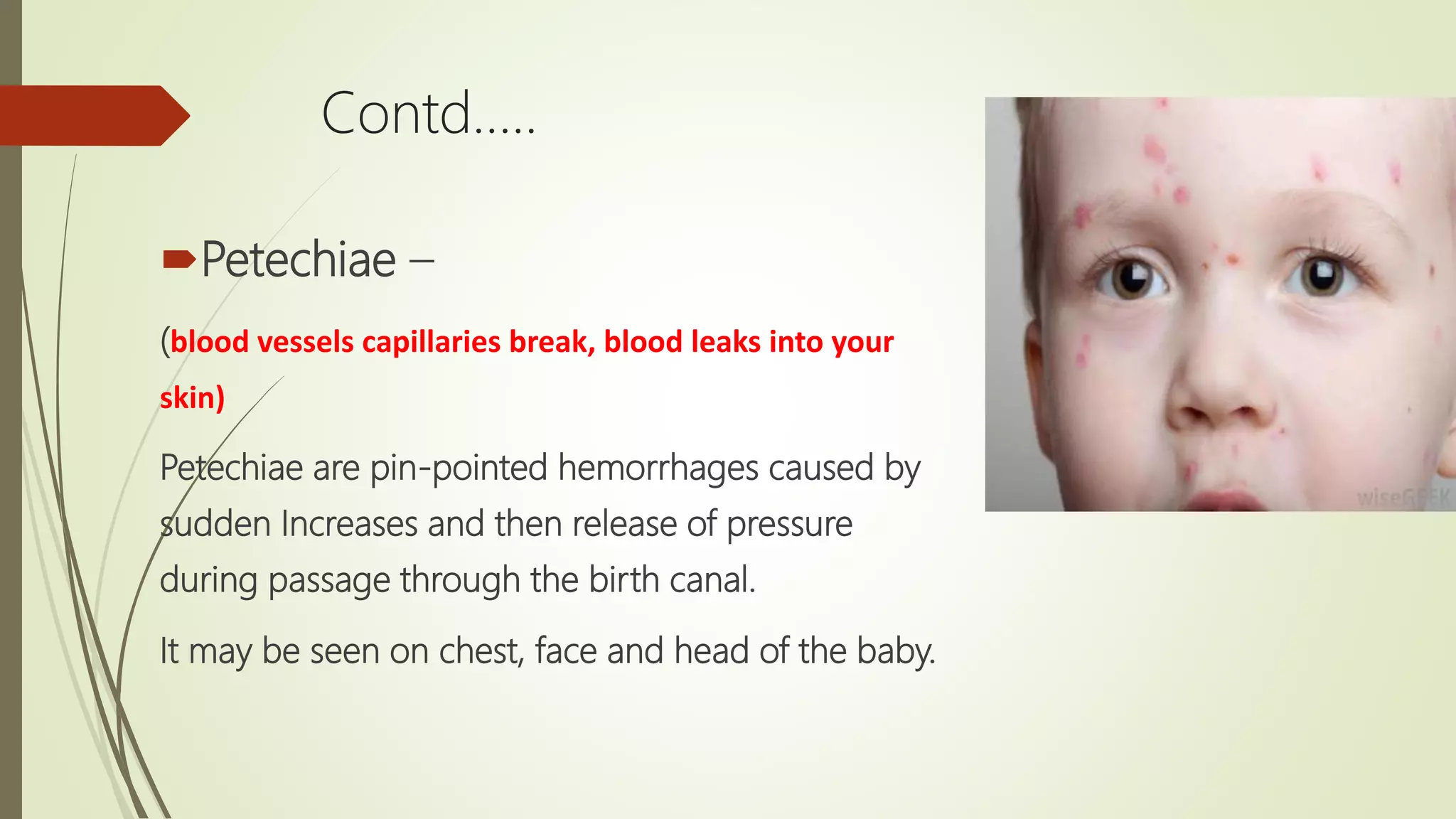
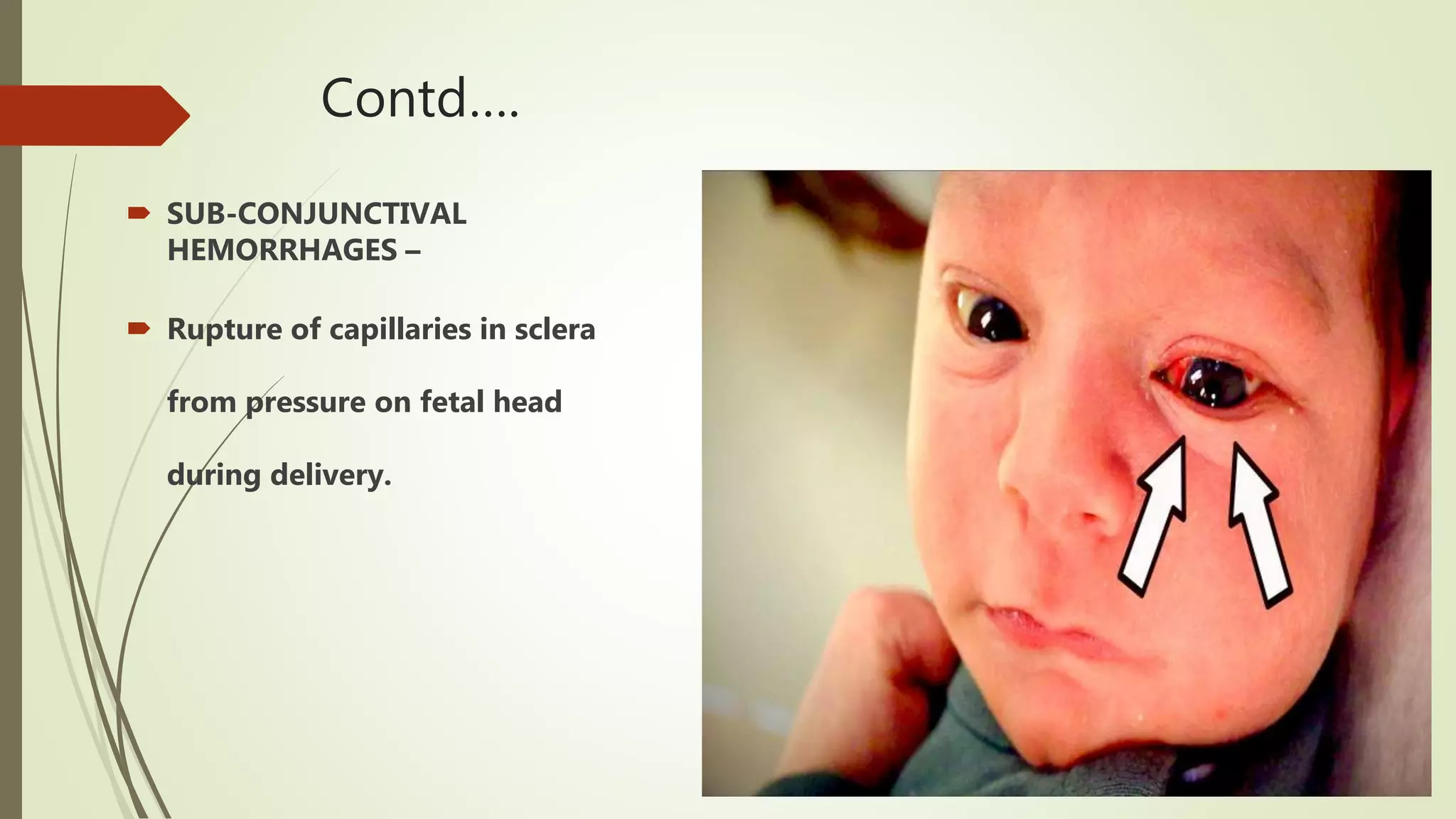
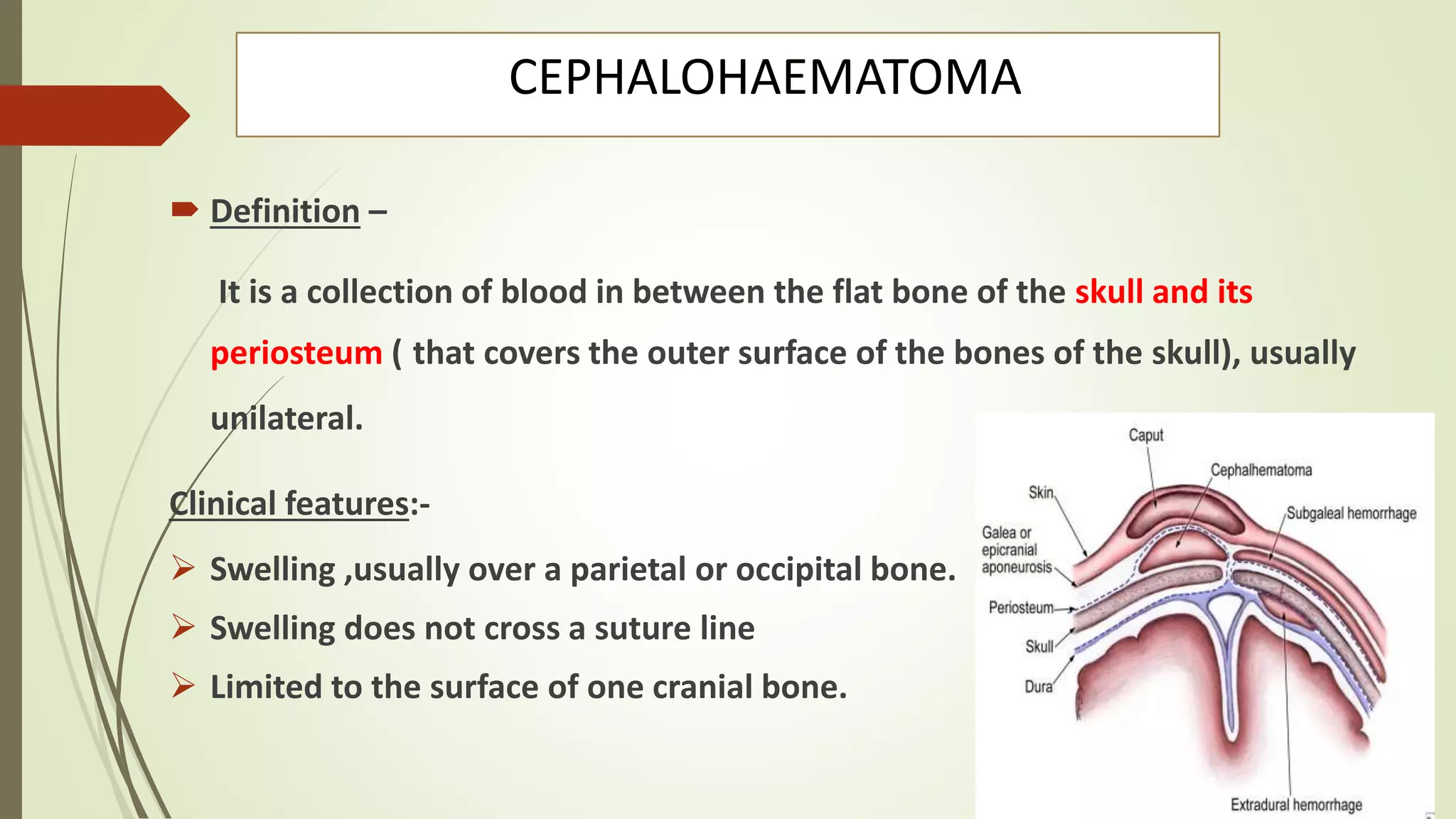
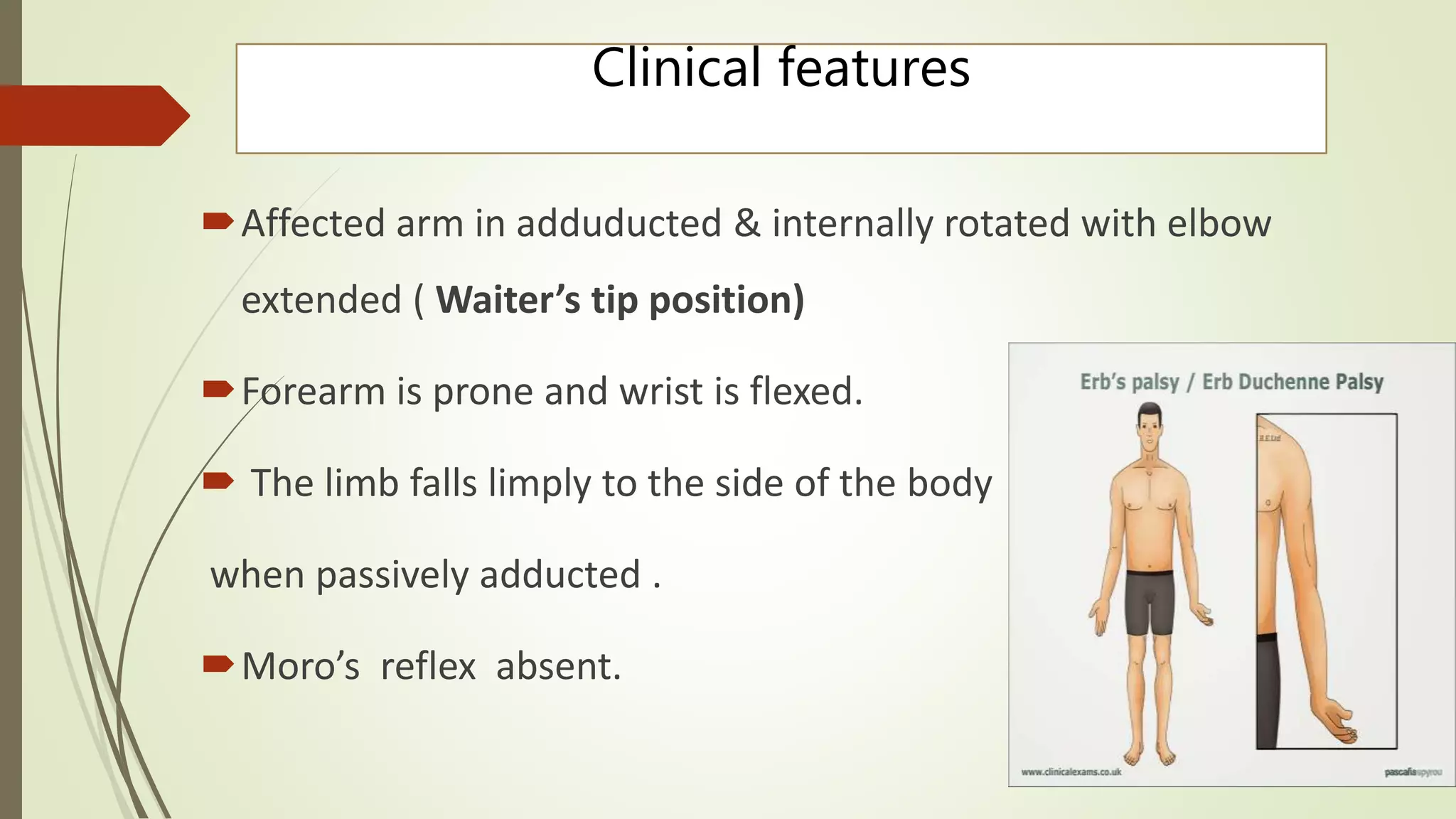
Common neonatal disorders include birth injuries, physiological problems, and respiratory, sepsis, and seizure issues. Birth injuries can involve soft tissue, the head, or nerves. Physiological problems include hyperbilirubinemia, hypoglycemia, hypocalcemia, and hypothermia. Respiratory disorders include respiratory distress syndrome and meconium aspiration syndrome. Neonatal jaundice is usually physiological but can also be pathological, breastfeeding-related, or due to breast milk. It is assessed and managed through history, examination, tests, phototherapy or admission based on bilirubin levels.