This document provides a summary of key points about various topics related to colon and lower gastrointestinal diseases:
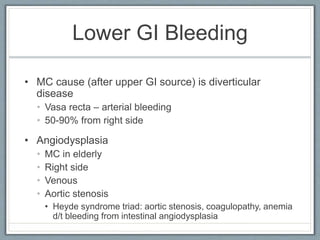
1) It discusses the anatomy and physiology of the colon, causes of ischemic colitis, treatments for Clostridium difficile and lower GI bleeding, and criteria for surgery for lower GI bleeding.
2) It reviews Ogilvie syndrome, sigmoid volvulus, cecal volvulus, diverticular disease, familial adenomatous polyposis, Lynch syndrome, Peutz-Jeghers syndrome, and inflammatory bowel diseases.
3) It covers screening recommendations, staging, treatment options for colon cancer and analyzes polyp types and criteria for surgery after polypectomy.