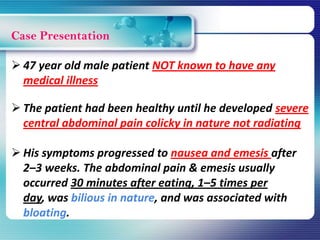
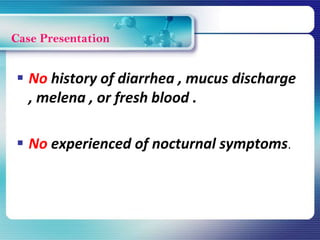
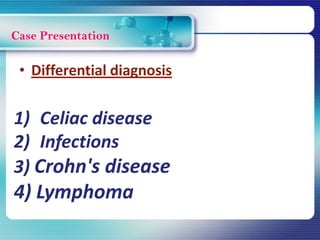
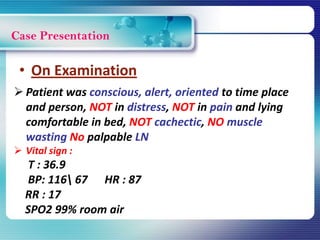
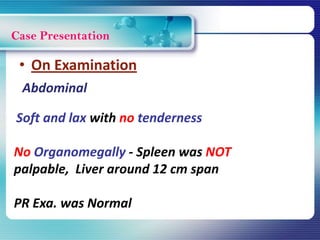
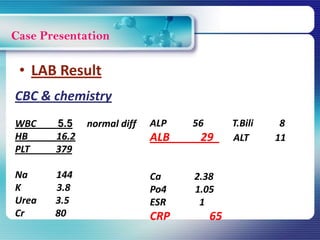
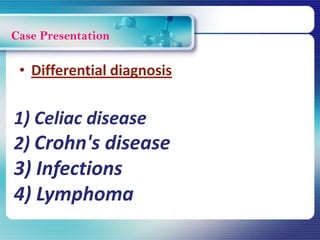
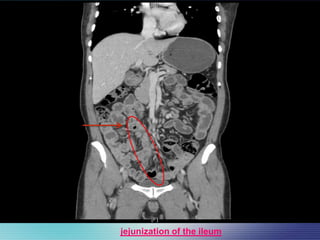
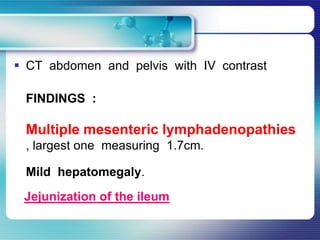
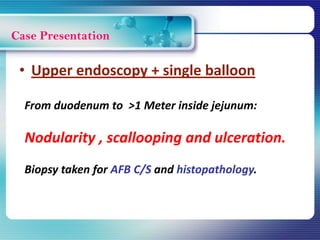
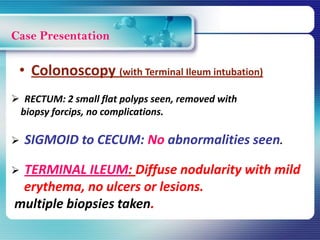
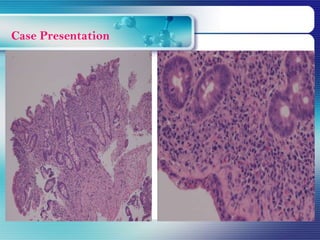
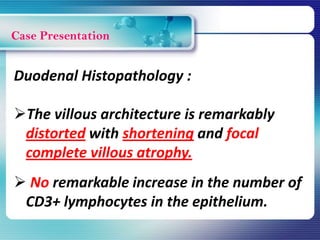
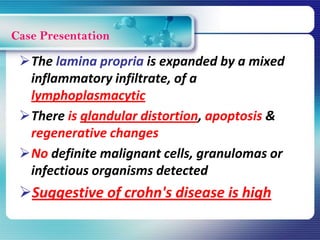
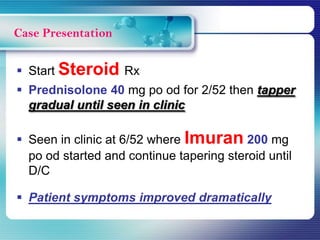
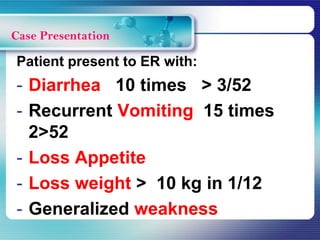
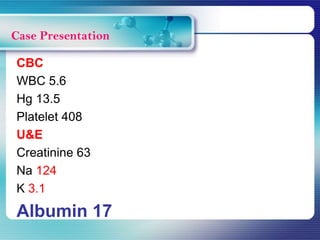
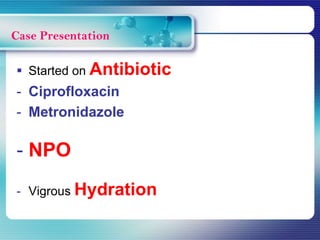
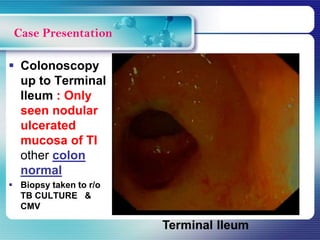
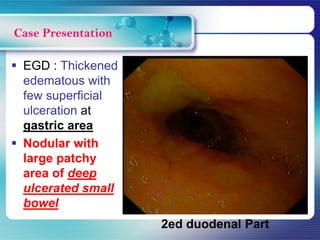
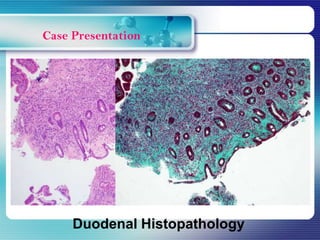
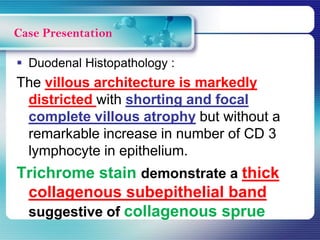
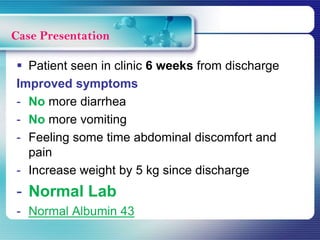
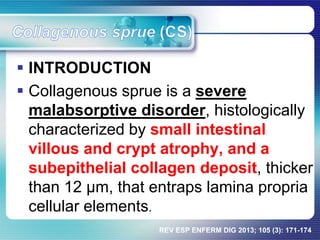
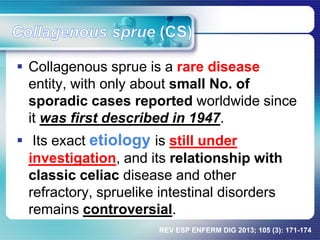
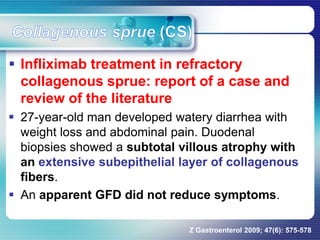
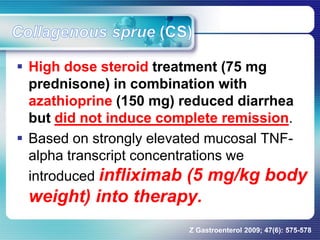
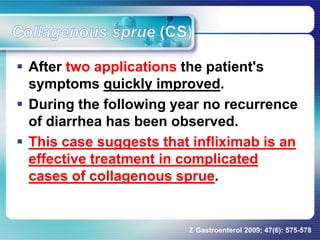
This case presentation discusses a 47-year old male patient who was referred for abdominal pain, nausea, vomiting and significant weight loss. Investigations revealed jejunization of the ileum on CT scan and villous atrophy on biopsy. The patient was initially treated for Crohn's disease but did not improve. Further histopathology found a thick collagenous band suggestive of collagenous sprue. The patient was started on a gluten-free diet, steroids, total parenteral nutrition, and anti-TNF therapy, leading to improved symptoms. Collagenous sprue is a rare malabsorptive disorder characterized by villous atrophy and thick subepithelial collagen deposits. Treatment is challenging but may include steroids