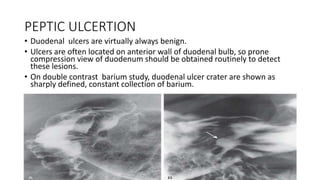
1. Duodenal ulcers are commonly located on the anterior wall of the duodenal bulb and can be detected on compression views of the duodenum. Complications include perforation, bleeding, and stenosis.
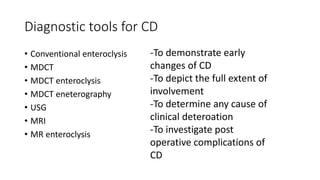
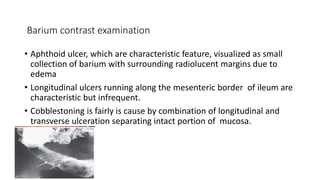
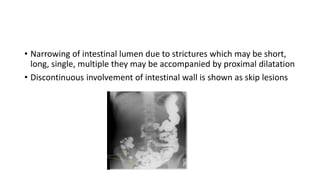
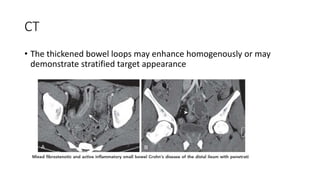
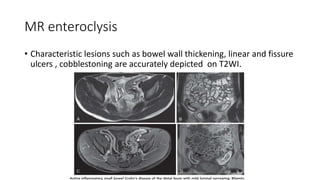
2. Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract. It is characterized on imaging as ulceration, cobblestoning, and strictures that can cause narrowing of the intestinal lumen.
3. Small bowel malignancies such as adenocarcinoma and carcinoid tumors often present as intraluminal masses that can cause concentric narrowing of the bowel wall and sometimes invade locally or metastasize distantly.