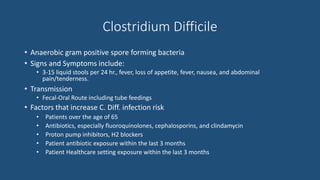
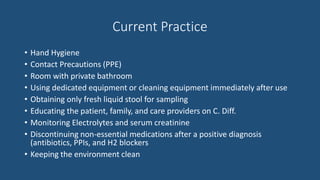
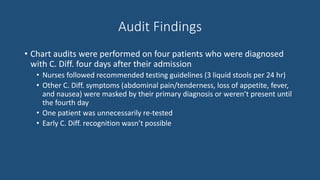
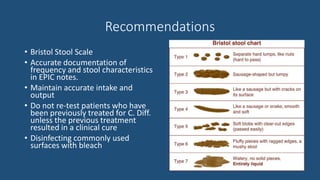
The document discusses Clostridium Difficile (C. Diff), a gram-positive, spore-forming bacteria that causes symptoms like diarrhea, fever, and abdominal pain. Risk factors for C. Diff infection include older age, antibiotic use, and recent healthcare exposure. Current practices to prevent and manage C. Diff involve hand hygiene, contact precautions, environmental cleaning, and discontinuing unnecessary medications after diagnosis. An audit found that in some cases, C. Diff symptoms were masked by primary diagnoses or developed later, preventing early recognition. Recommendations include using a stool scale to document symptoms accurately and maintaining intake/output records to help with early detection and management of C. Diff.
![References
• "Health Professional Information on Clostridium Difficile." Minnesota Department of Health.
2015. Retrieved from http://www.health.state.mn.us/divs/idepc/diseases/cdiff/hcp/index.html
• Bor, B. Clostridium Difficile [Powerpoint]
• "Bristol Stool Chart." Continence Foundation of Australia. 2016. Retrieved from
http://www.continence.org.au/pages/bristol-stool-chart.html
• “Clostridium Difficile Infection (CDI) Prevention Strategies 2.0.” Collaborative Healthcare-
Associated Infection Network. Retrieved from
http://www.mnreducinghais.org/documents/HAIGapAnalysisCDI.PDF](https://image.slidesharecdn.com/clostridiumdifficilepowerpointpresentation-161127183925/85/Clostridium-difficile-powerpoint-presentation-6-320.jpg)