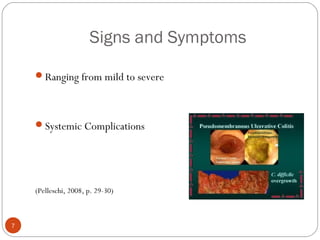
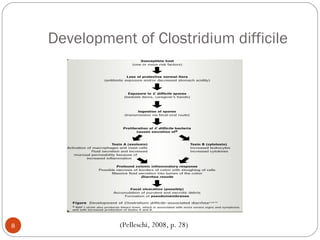
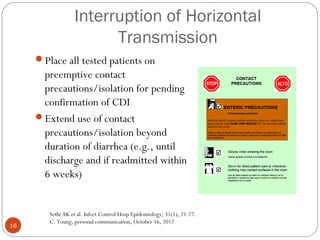
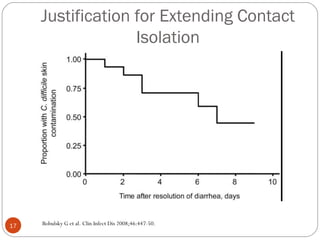
This document discusses Clostridium difficile (C. difficile) infection, including that it affects 40% of patients in hospital settings, surpasses MRSA infections, and is transmitted through the fecal-oral route. Risk factors include antibiotic use, advanced age, and recent surgery or chemotherapy. Signs and symptoms range from mild to severe diarrhea and systemic complications. Prevention strategies discussed include hand hygiene, contact precautions, environmental cleaning, and antibiotic stewardship.