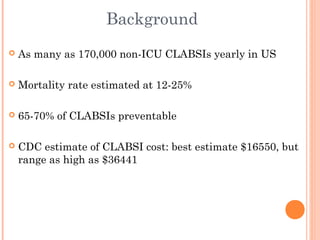
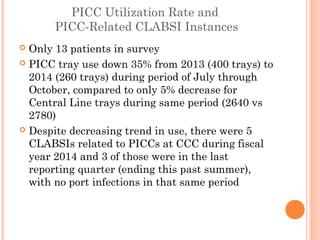
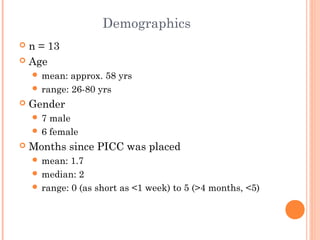
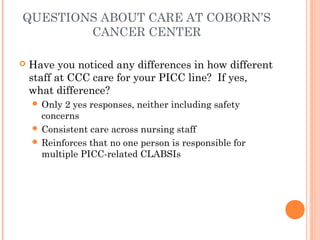
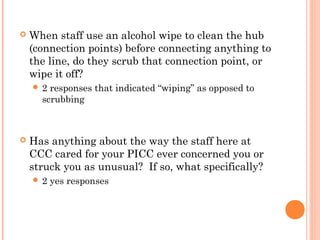
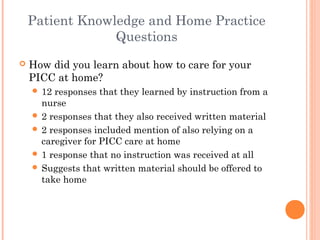
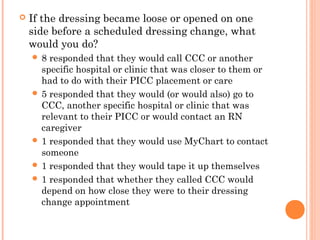
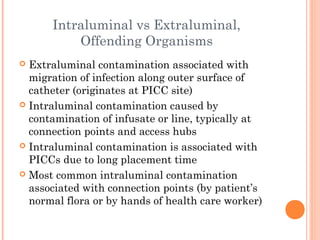
This document summarizes a presentation about eliminating central line-associated bloodstream infections (CLABSIs) in patients with peripherally inserted central catheters (PICCs) at Coborn's Cancer Center. A survey of 13 PICC patients found that while PICC tray use had decreased, there were still 5 CLABSIs related to PICCs in the previous year. The survey also assessed patient knowledge of PICC care and found room for improvement in educating patients about signs of infection. The presentation recommends frequent re-education of patients and caregivers on PICC care best practices such as hand hygiene and hub disinfection to help further reduce CLABSI rates.
![References
Krook, J., Steinmann, K. (2014). Crashing Through the Barriers to
CLABSI Prevention [PowerPoint document].
www.mmicgroup.com/resources/webinars/upcoming/542-upcoming-crashing-
through-the-barriers+&
cd=3&hl=en&ct=clnk&gl=us&client=firefox-a
Moureau, N., Dawson, R. (2010). Keeping needleless connectors clean,
part 1. Nursing: May 2010, 40(5), 18–19.
doi: 10.1097/01.NURSE.0000371119.85145.99
Tavianini, H., Deacon, V., Negrete, J., Salapka, S. (2014). Up for the
challenge: Eliminating peripherally inserted central catheter
infections in a complex patient population. Journal of the Association
for Vascular Access, 19(3), 159-164.
Taylor, C., Lillis, C, LeMone, P., Lynn, P. (2011). Fundamentals of
nursing: the art and science of nursing care, 7th edition. Philadelphia,
PA: Lippincott, Williams & Wilkins.
The Joint Commission. (May, 2012). Preventing central line–
associated bloodstream infections: A global challenge, a global
perspective. Oak Brook, IL: Joint Commission Resources.
http://www.PreventingCLABSIs.pdf](https://image.slidesharecdn.com/piccclabsipreventioncccfinal-141210231247-conversion-gate01/85/CLABSI-Prevention-19-320.jpg)