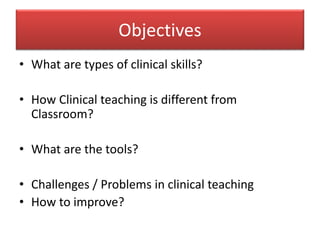
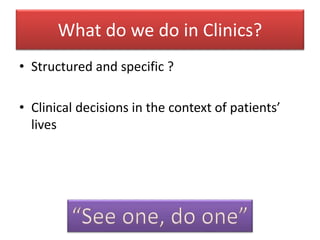
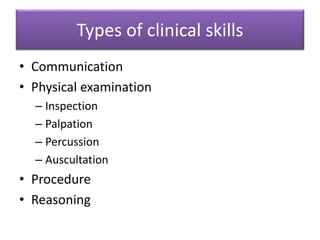
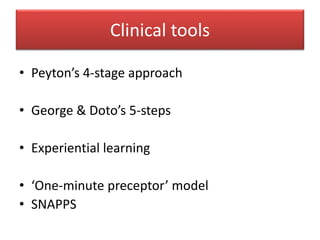
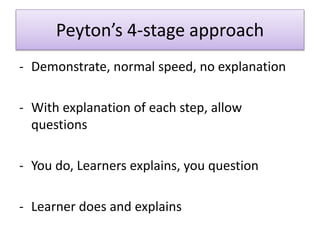
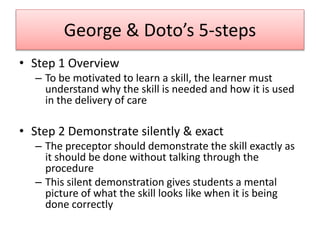
The document outlines the objectives and types of clinical skills necessary for effective clinical teaching, contrasting it with traditional classroom education. It details various teaching tools, including Peyton's 4-stage approach and George & Doto’s 5-steps, emphasizing experiential learning and active student involvement. Challenges such as time pressures and lack of clear objectives are presented, alongside suggestions for improving clinical teaching practices to foster competent, independent, and critical-thinking practitioners.