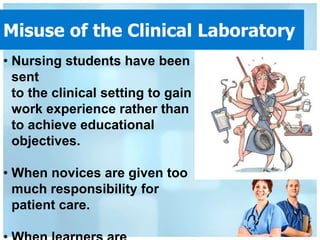
Clinical teaching provides opportunities for nursing students to apply theory in practice settings. It aims to develop students' skills, problem-solving, and cultural competence. Traditional models involve instructors accompanying groups of students who are assigned patients. Preceptorship models pair a student with a practicing nurse for supervision and guidance.
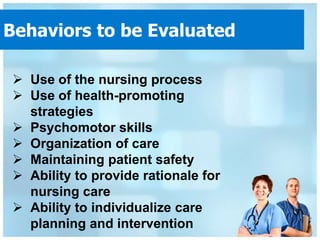
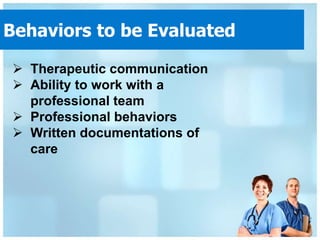
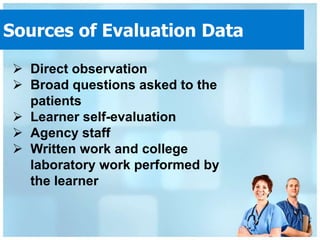
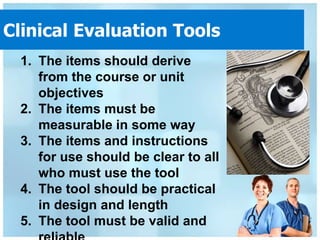
Effective clinical instruction requires preparation like selecting sites, identifying units, and arranging student assignments. During sessions, preconferences orient students and postconferences allow analysis and evaluation. Formative and summative evaluations provide feedback and assess competencies in areas like critical thinking and documentation. Evaluation tools must be clear, measurable, and practical for improving student learning in clinical placements.