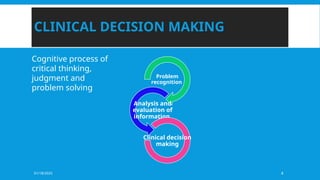
The document discusses the complex process of clinical decision-making in physiotherapy, emphasizing the importance of critical thinking, evidence-based practice, and effective communication skills in patient care. It outlines the frameworks and models used in clinical reasoning, including the International Classification of Functioning (ICF) and the patient management model, which guides physiotherapists in evaluating and addressing patients' needs. Additionally, it includes a detailed case study illustrating the application of these frameworks in developing a treatment plan for a patient with motor function impairments due to a traumatic brain injury.