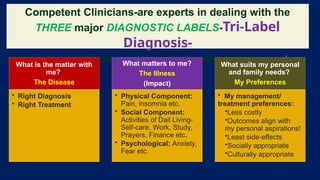
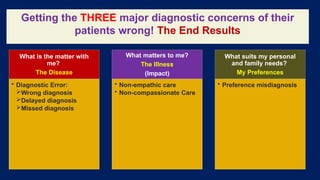
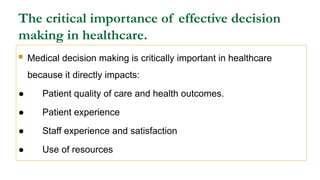
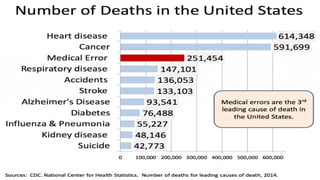
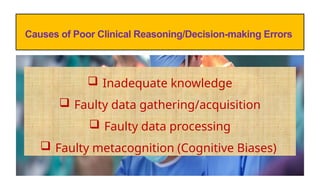
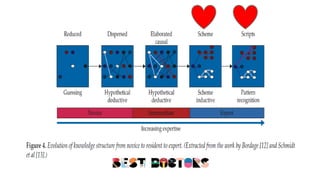
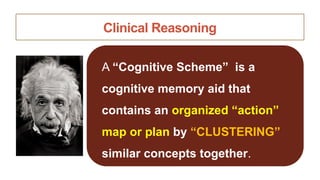
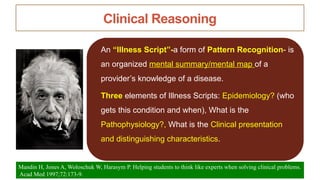
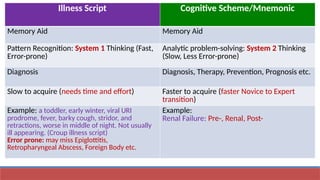
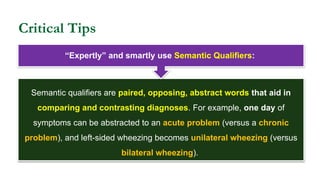
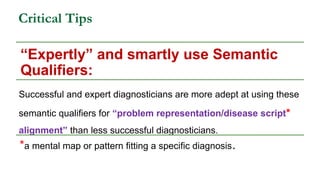
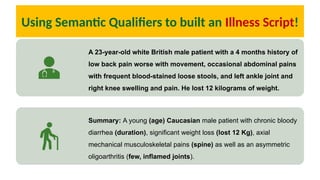
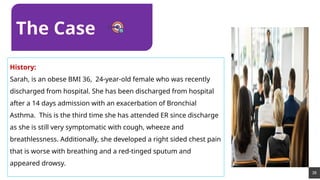
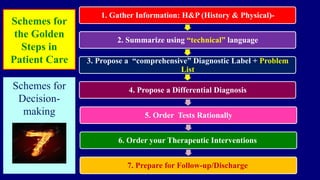
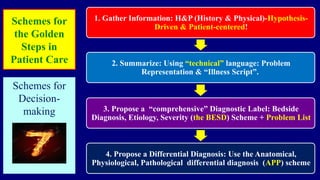
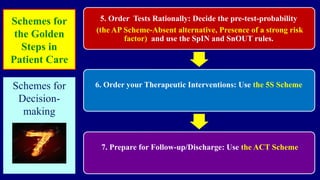
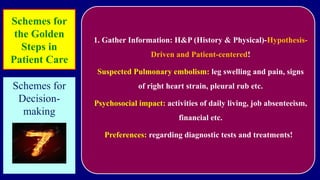
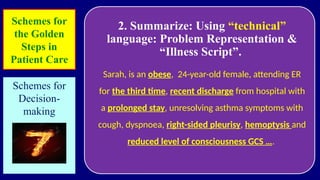
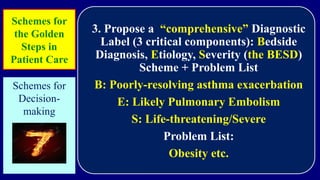
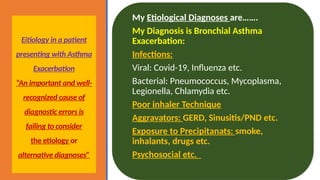
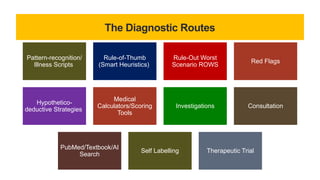
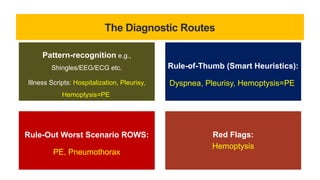
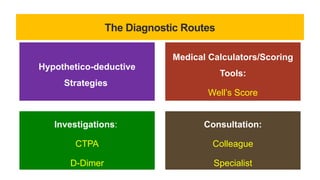
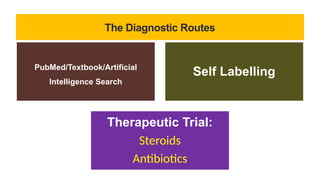
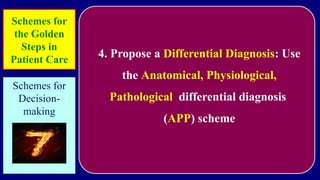
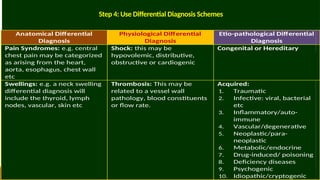
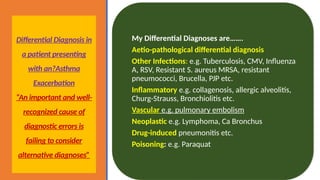
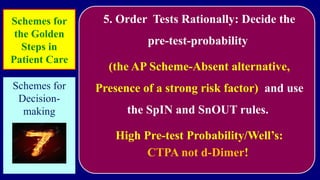
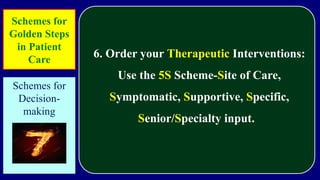
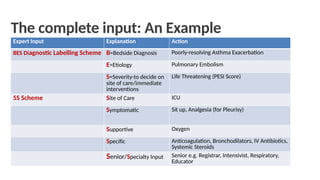
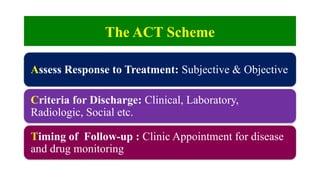
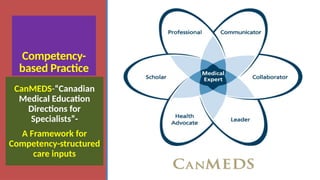
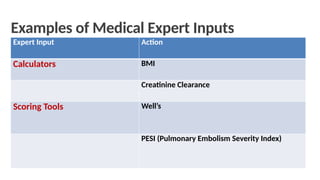
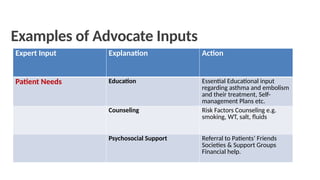
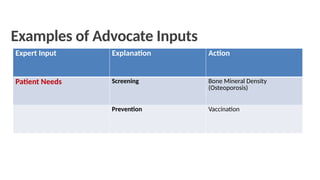
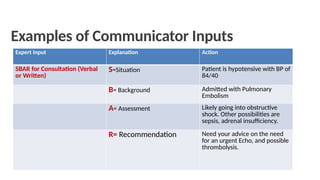
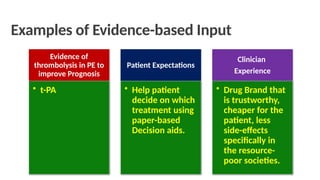
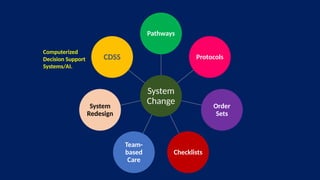
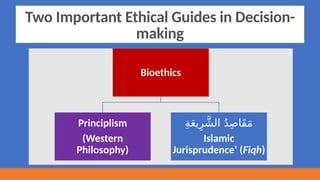
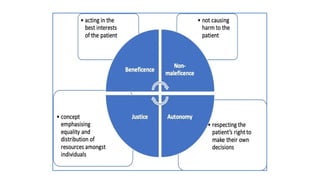
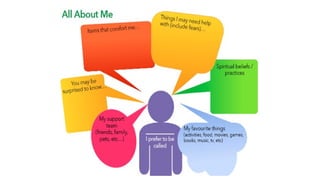
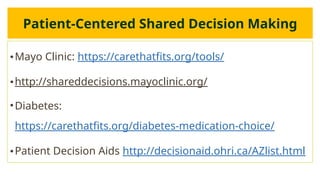
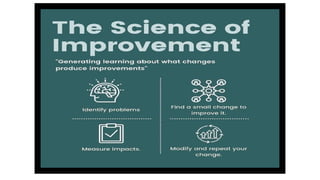
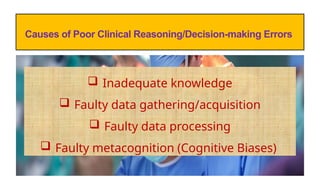
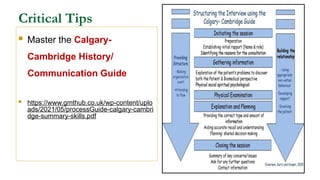
The document outlines advanced concepts in medical decision-making and critical thinking, emphasizing a competence-by-design approach to train healthcare professionals. It discusses the importance of integrating cognitive schemes, diagnostic routes, and patient-centered care in clinical practice. Additionally, it highlights the necessity for effective decision-making to enhance patient quality of care and avoid diagnostic errors.