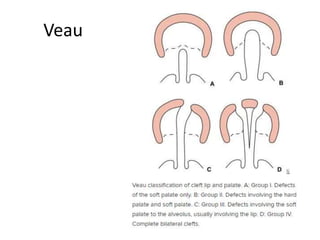
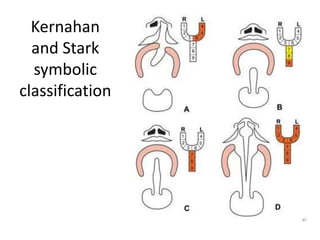
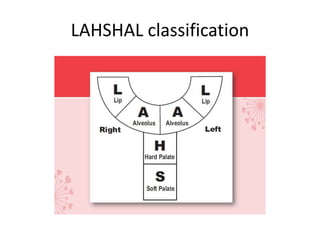
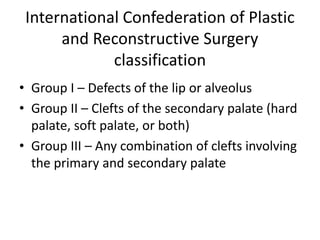
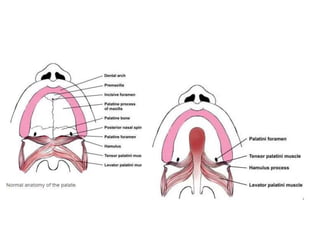
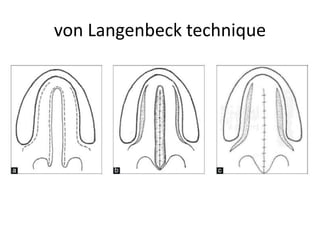
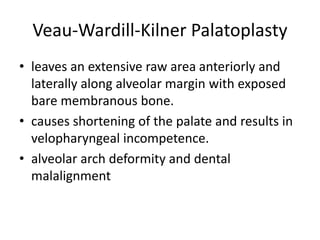
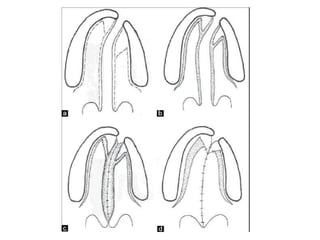
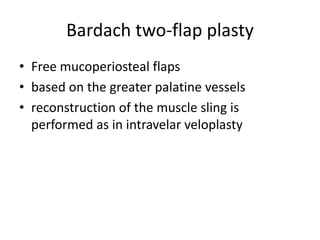
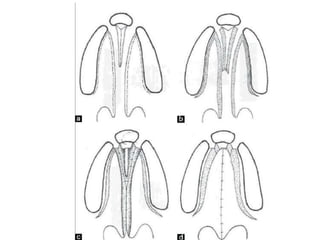
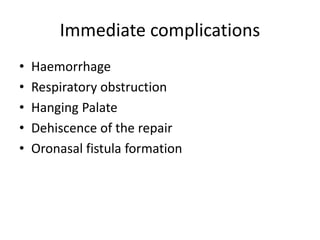
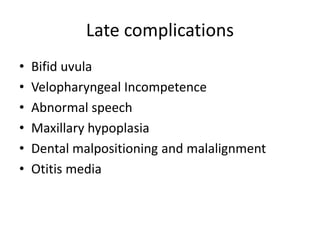
This document discusses classifications and repair techniques for cleft palate. It describes three main groups of cleft palate classifications based on the location and extent of the cleft. For repair, it recommends timing of 12-18 months when babbling occurs. Key principles of repair include closure of the defect, reconstruction of the muscle sling, and retropositioning of the soft palate. Several surgical techniques are outlined, including von Langenbeck's, Veau-Wardill-Kilner, Bardach's two-flap, and Furlow Double Opposing Z-Plasty methods. Post-operative care and potential complications are also reviewed.