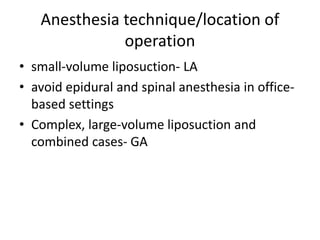
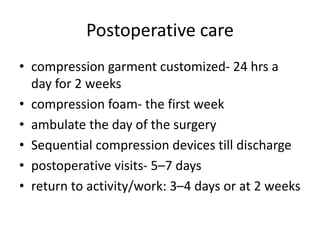
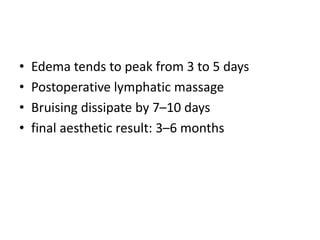
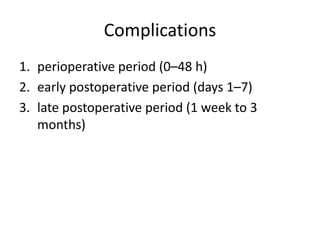
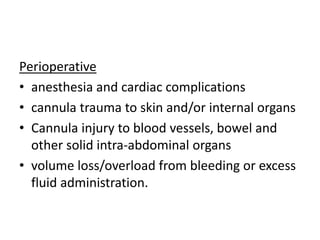
Liposuction is a surgical procedure to remove unwanted fat deposits from beneath the skin. It was originally introduced in the 1980s and involves using suction to aspirate fat through small incisions. There are several techniques including traditional suction-assisted liposuction, ultrasound-assisted, power-assisted, vaser-assisted, and laser-assisted liposuction. Patient selection, pre-operative evaluation and planning, anesthesia technique, and post-operative care are important considerations to achieve optimal results and avoid complications from liposuction.