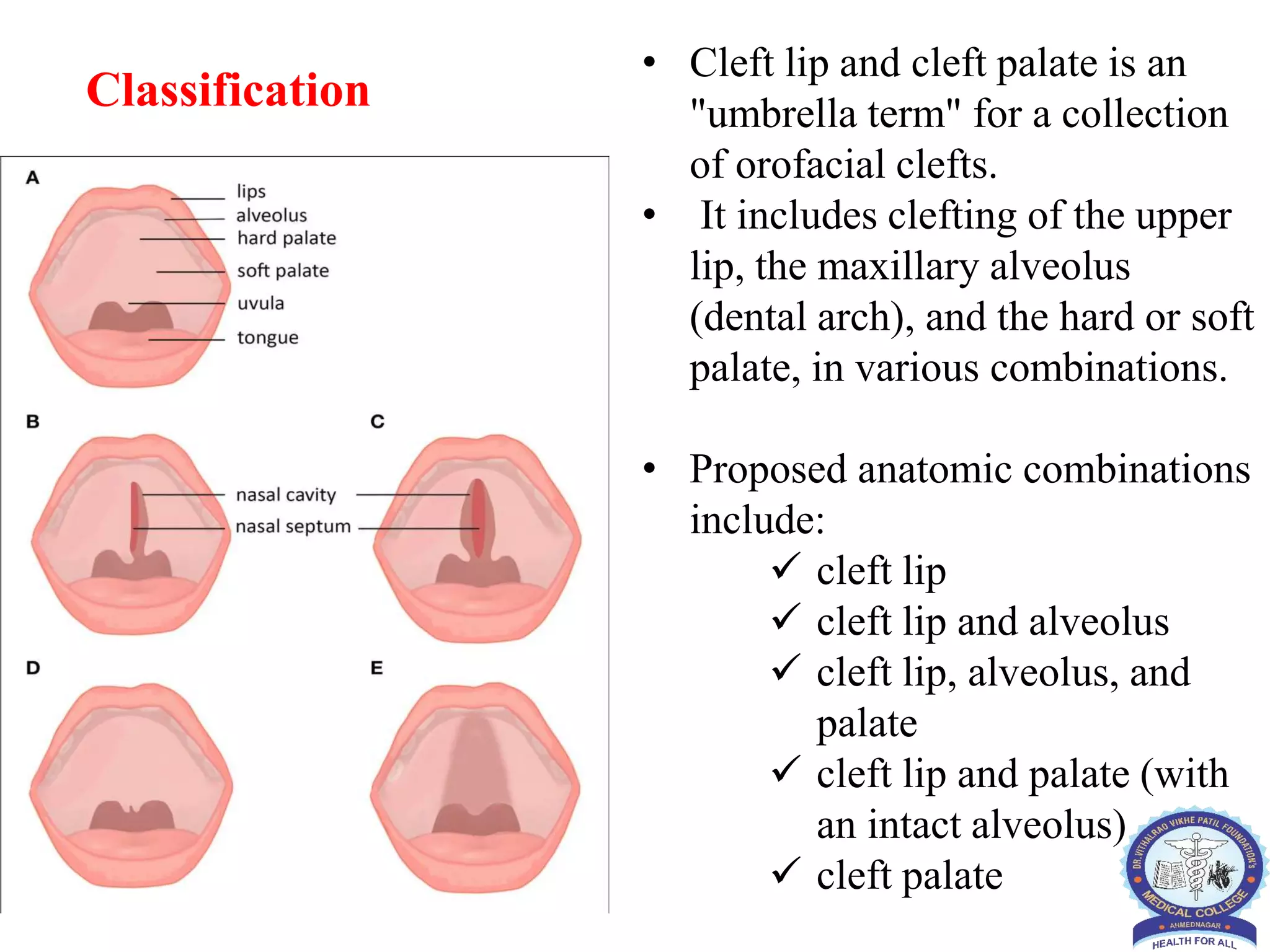
This document provides information about cleft lip and cleft palate including causes, risk factors, diagnosis, treatment, and social aspects. It describes how cleft lip occurs when the tissues of the lip do not fully fuse before birth, and cleft palate occurs when the roof of the mouth does not fully close. Treatment often begins in infancy and may include surgery, dental care, speech therapy, and psychological support. The document also discusses cultural beliefs and stigma around cleft conditions as well as organizations providing cleft care in India.