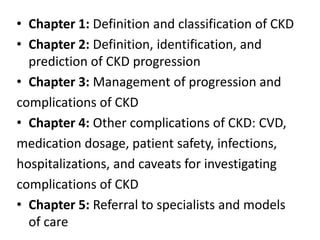
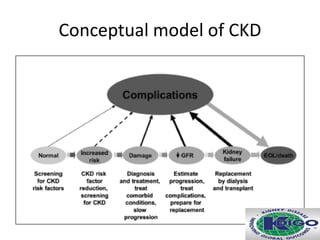
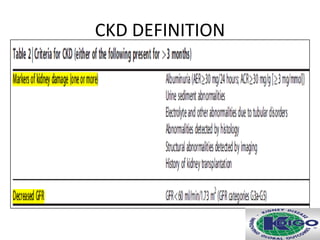
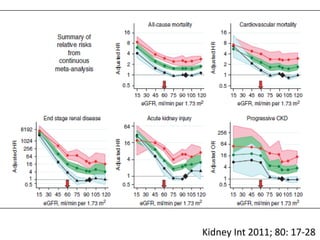
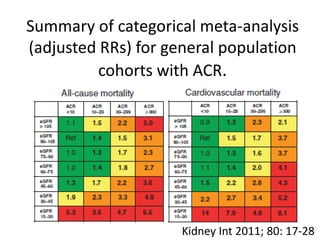
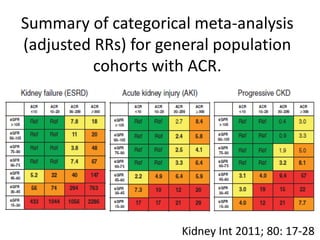
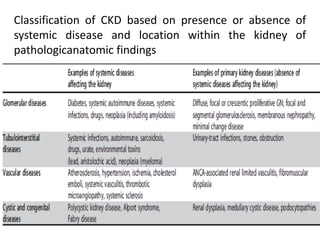
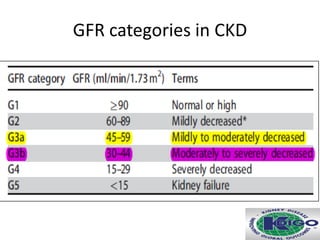
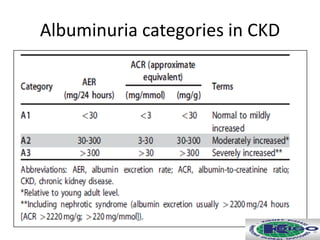
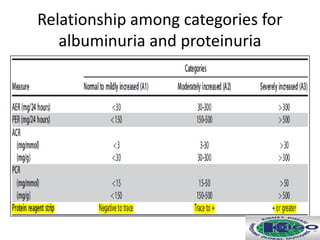
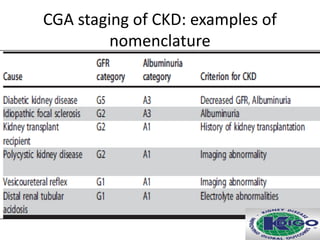
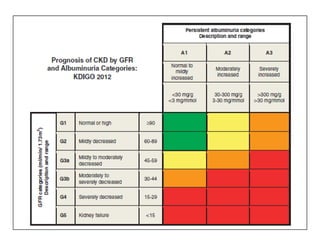
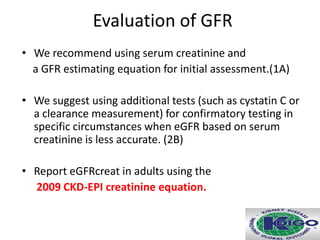
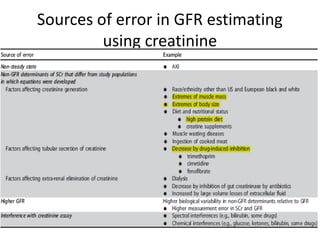
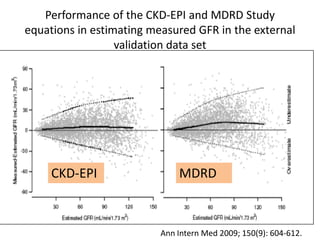
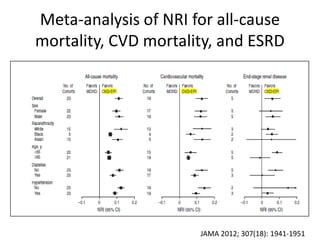
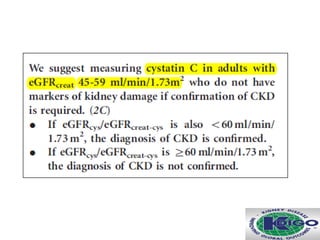
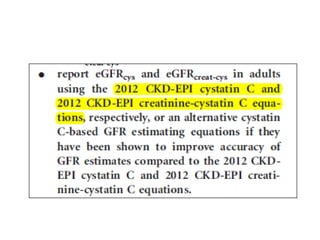
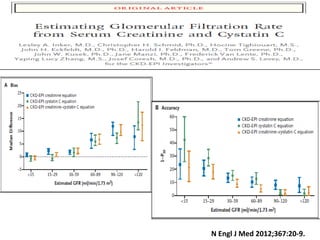
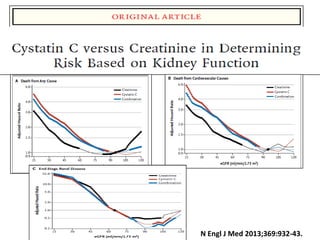
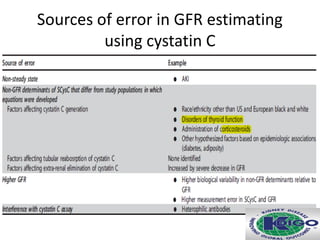
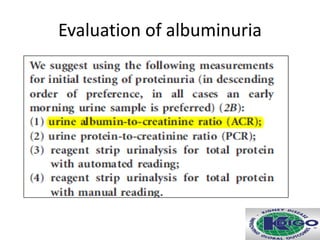
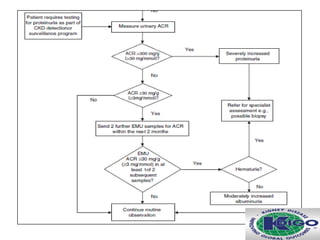
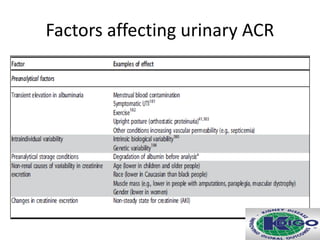
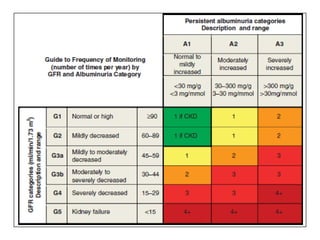
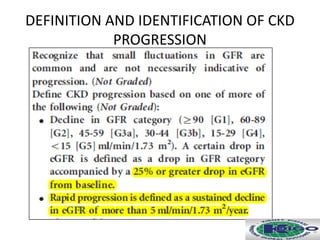
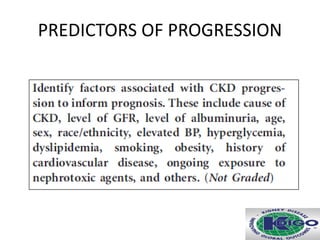
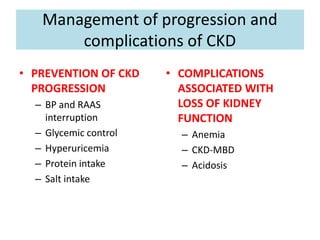
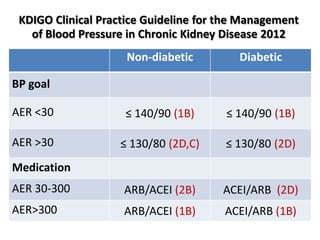
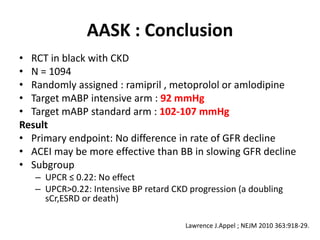
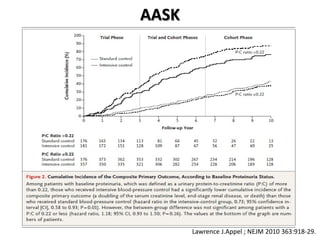
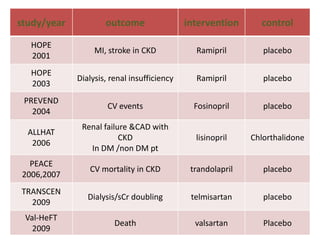
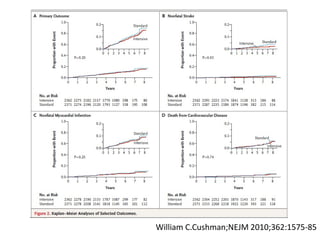
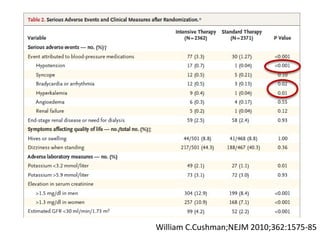
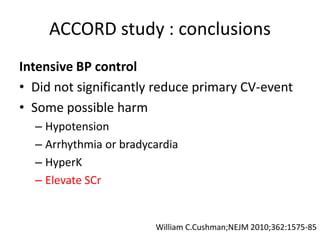
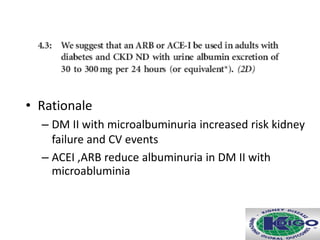
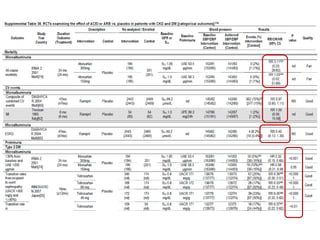
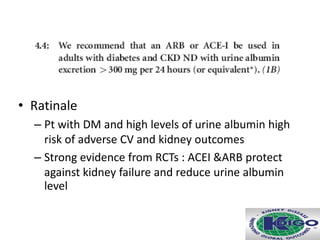
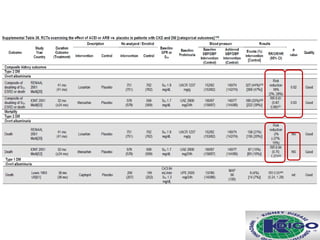
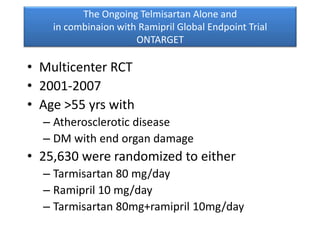
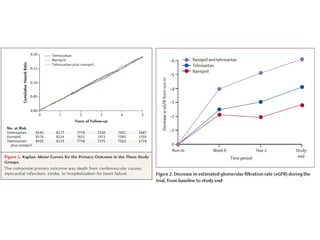
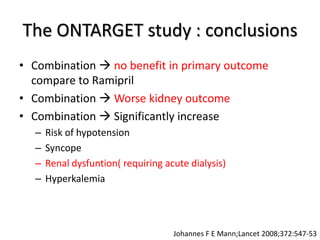
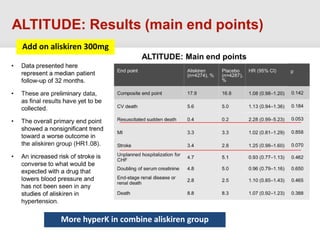
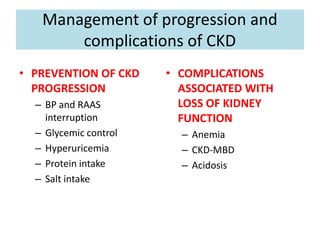
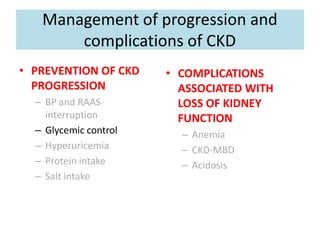
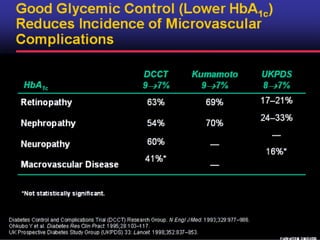
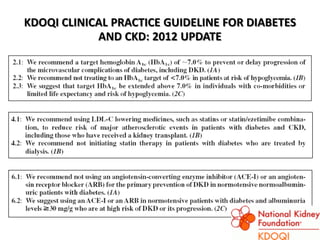
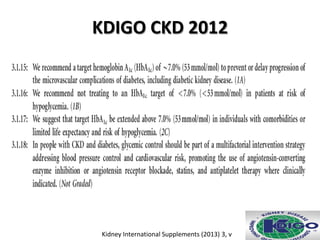
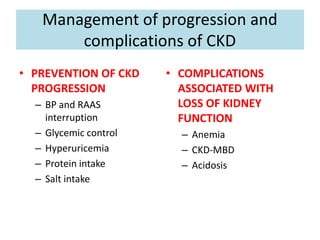
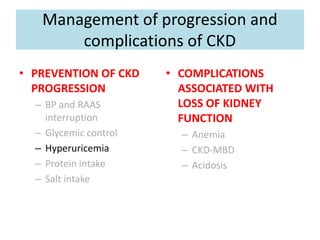
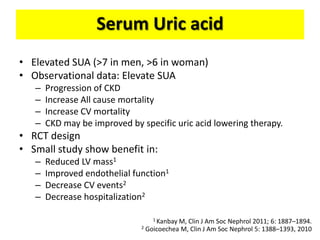
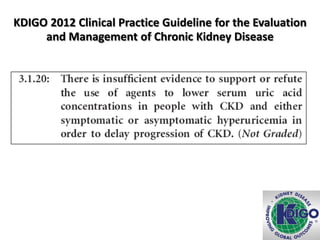
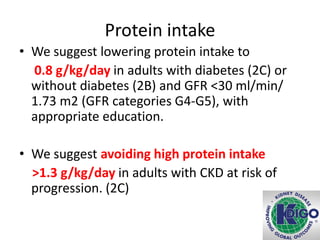
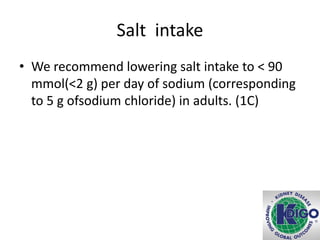
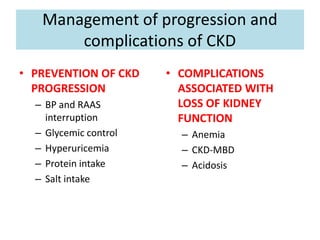
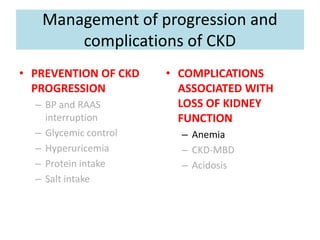
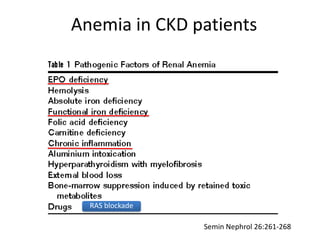
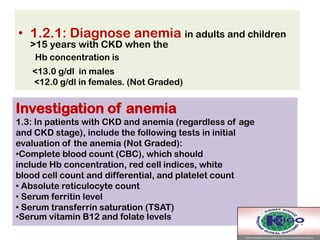
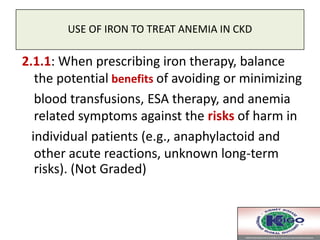
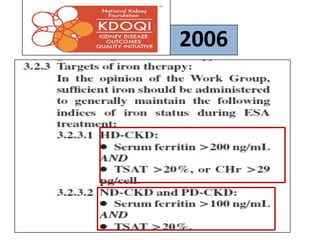
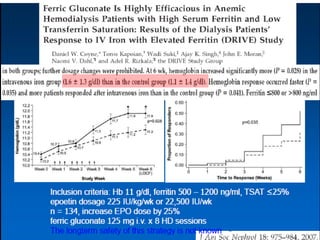
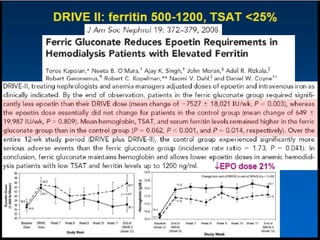
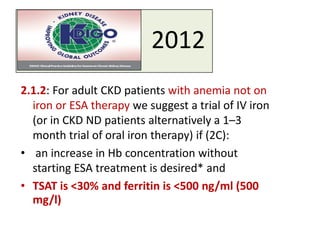
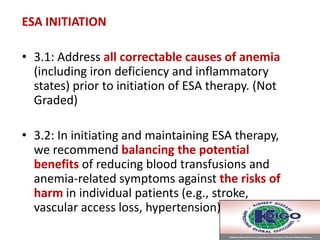
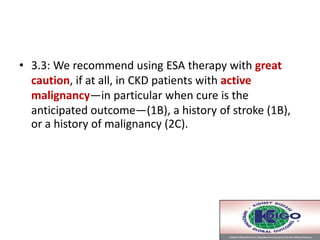
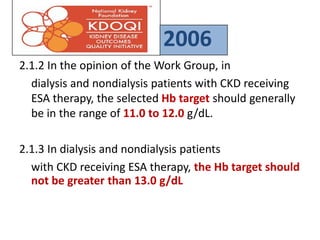
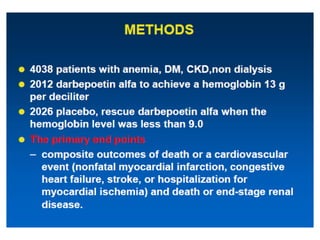
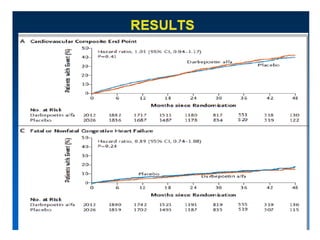
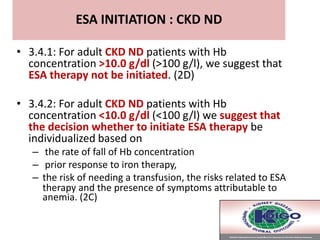
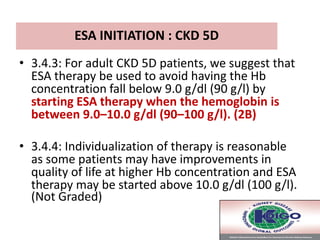
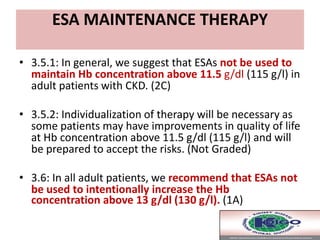
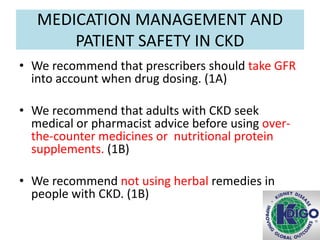
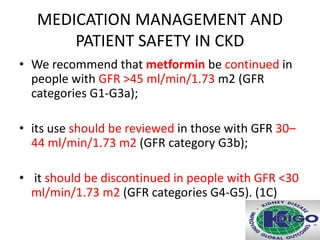
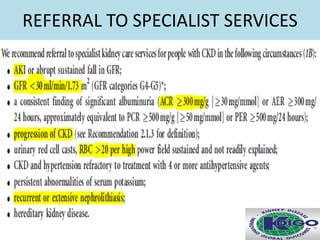
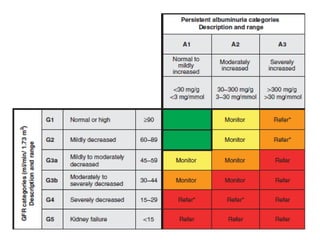
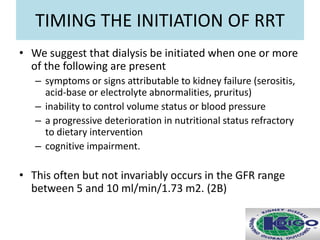
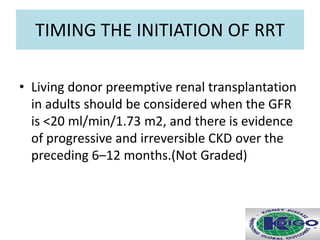
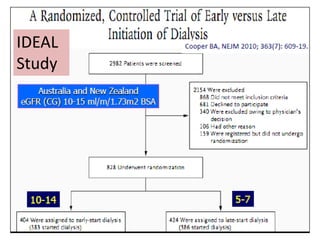
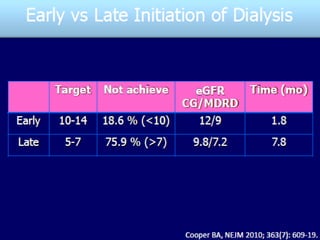
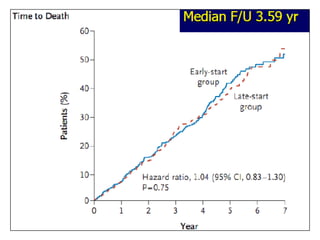
The document summarizes chronic kidney disease (CKD) and its management. It defines CKD and outlines the new classification system. It discusses evaluating kidney function through estimated GFR and albuminuria. It covers managing CKD progression through blood pressure control, RAAS interruption, glycemic control, and treating complications like anemia. It recommends lowering protein intake in later stages and salt intake. Overall, the document provides clinical practice guidelines for defining, evaluating, and managing CKD and its progression and complications.