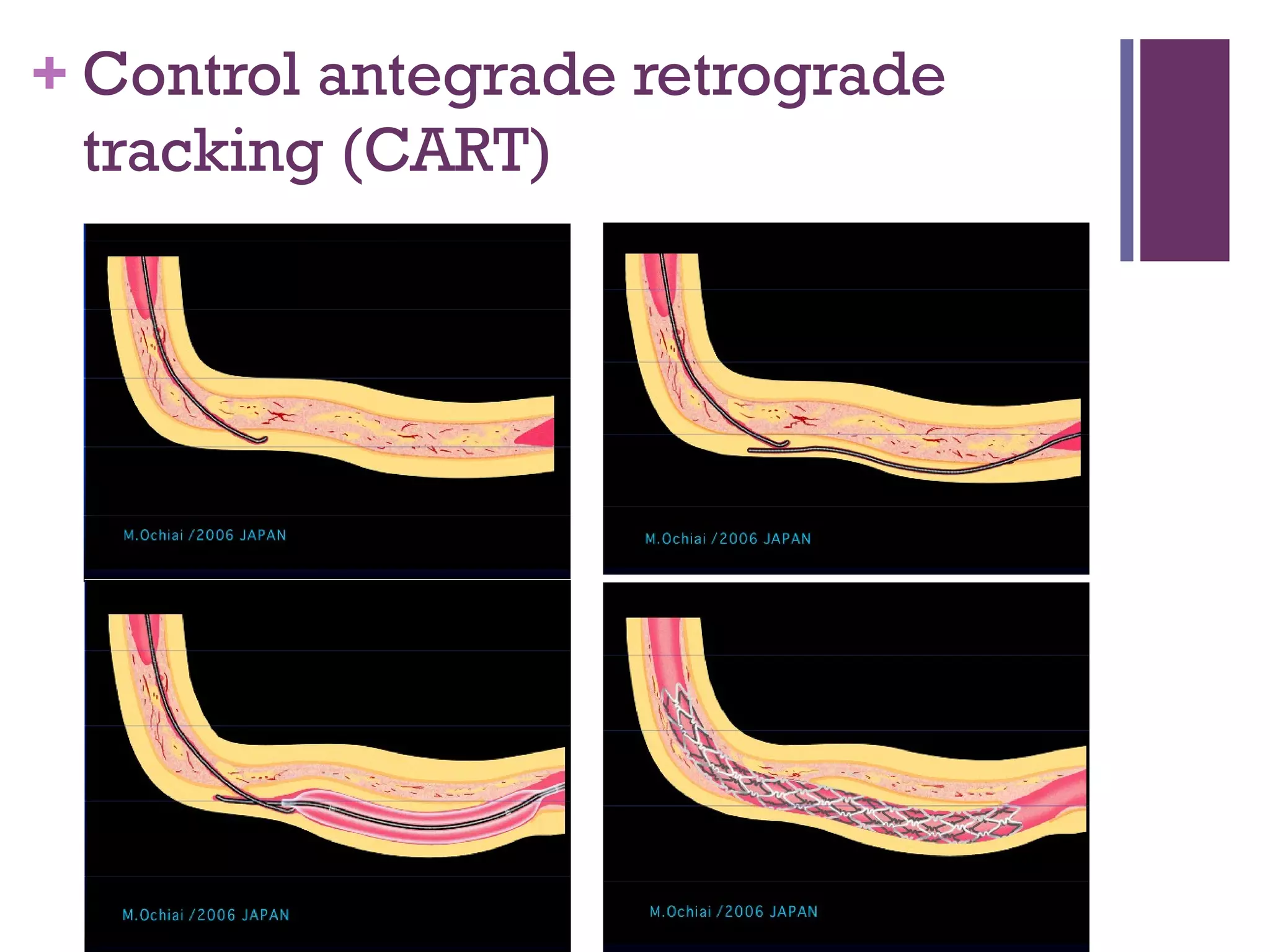
A 56-year-old male with a history of heart disease presented with ongoing chest pain after an unsuccessful attempt to open a chronic total occlusion of the right coronary artery via percutaneous coronary intervention 6 weeks prior. The patient underwent a second PCI procedure where the CTO was successfully opened using an antegrade approach, resolving his symptoms. At follow-ups 6 months, 12 months and 18 months later, the patient reported continued relief from symptoms and was able to return to exercising and training for triathlons without any chest pain.