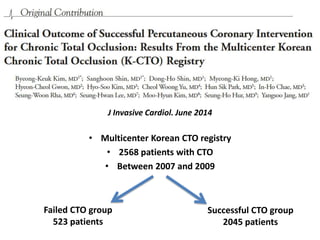
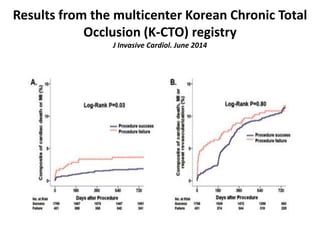
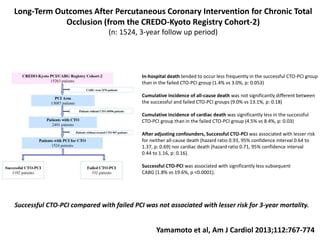
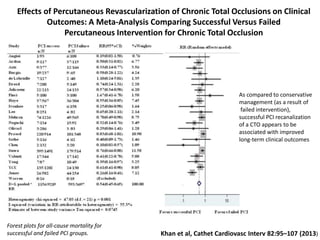
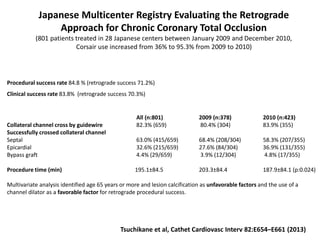
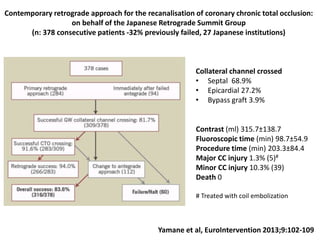
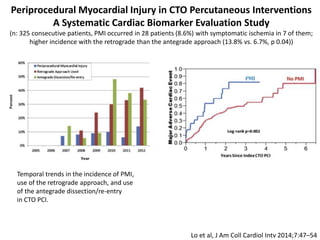
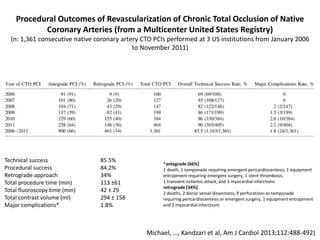
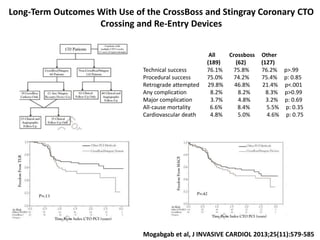
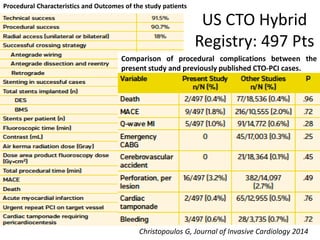
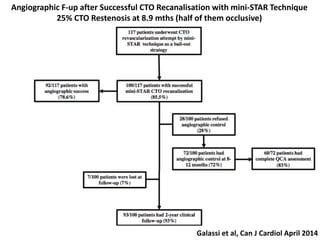
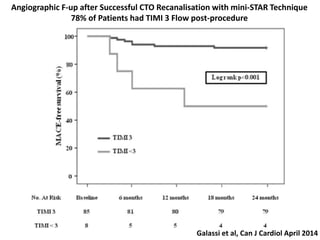
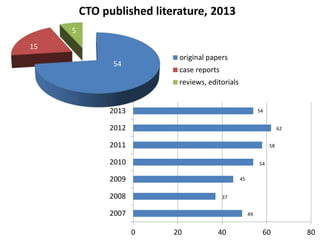
- Recent publications on CTOs from 2013-2014 focused on pathology, physiology, epidemiology, outcomes, imaging, technical approaches, and stents.
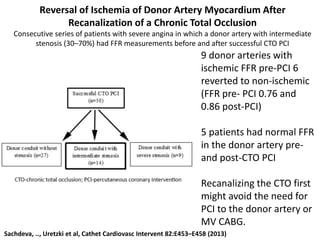
- Studies showed differences in plaque characteristics between long and short duration CTOs and impact of revascularizing CTOs on donor arteries.
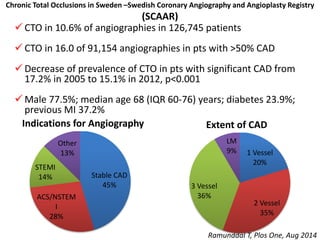
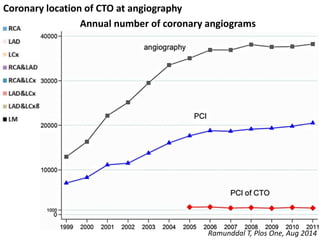
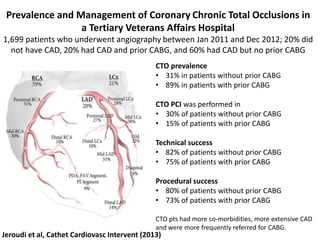
- Registry data from Sweden found a 10.6% prevalence of CTOs and decreasing rates over time.
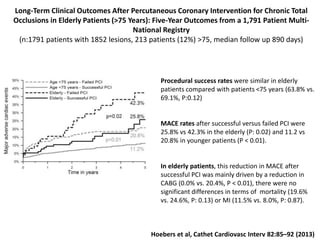
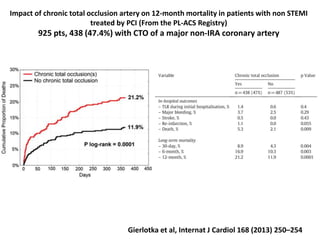
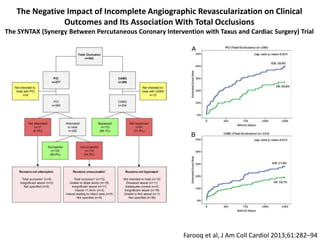
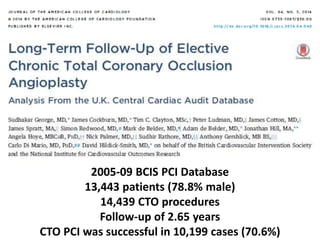
- Successful CTO PCI was associated with improved survival, less cardiac death, and reduced need for CABG compared to failed procedures.
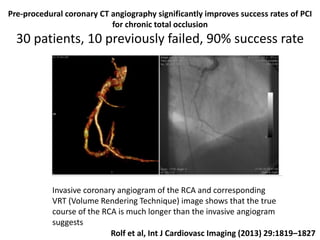
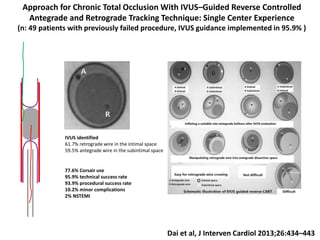
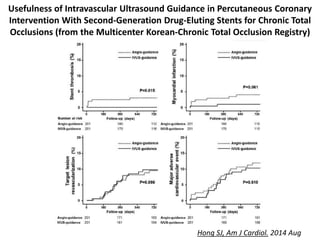
- Imaging like IVUS and CT angiography improved technical success rates for CTO PCI.

![Sakamura, …, Virmani et al, Eur Heart J. 2013 Oct 14
Comparison of pathology of chronic total occlusion
with and without coronary artery bypass graft
95 CTOs from 82 patients were divided into CTO with CABG(n:34) ,CTO without CABG—of
long-duration (n:49) and short-duration (n:12); histopathological comparison of the
plaque characteristics of CTO, proximal and distal lumen morphology, and negative
remodeling between groups; a total of 1127 sections were evaluated
Representative images of long-duration CTO and short-
duration CTO
Differences in plaque characteristics
• necrotic core area was highest in SD CTO
(18.6%) (LD-CTO: 7.8%; CTO+CABG: 4.5%; P ¼ 0.02)
• calcified area was greatest in CTO+CABG
(29.2%) (LD-CTO: 16.8%; SD-CTO: 12.1%; P ¼ 0.009);
• negative remodeling was least in SD-CTO
[remodeling index (RI) 0.86] [CTO+CABG (RI): 0.72
and LD-CTO (RI): 0.68; P , 0.001]
• Approximately 50% of proximal lumens
showed characteristics of abrupt closure
• the majority of distal lumen patterns were
tapered(79%) (P , 0.0001).](https://image.slidesharecdn.com/gendertfinaldimario-150910102747-lva1-app6892/85/08-25-Di-Mario-Recent-Pubblications-and-Research-4-320.jpg)
![Survival and CTO Success
• Successful PCI of at least 1 CTO was associated with improved survival (hazard ratio [HR]:
0.72; 95% CI: 0.62 to 0.83; p < 0.001)
Sudhakar et al. J Am Coll Cardiol. 2014;64:235-243](https://image.slidesharecdn.com/gendertfinaldimario-150910102747-lva1-app6892/85/08-25-Di-Mario-Recent-Pubblications-and-Research-15-320.jpg)