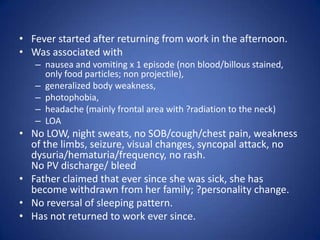
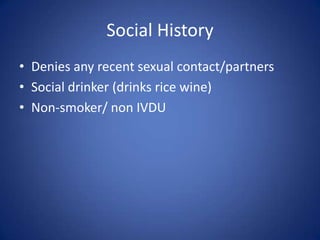
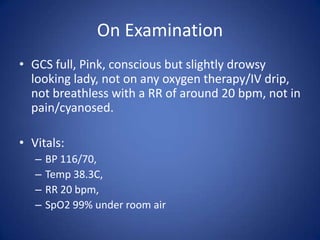
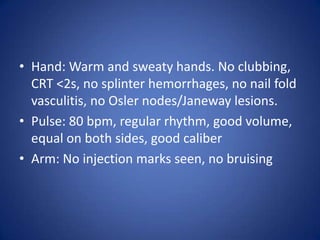
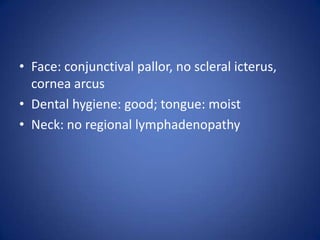
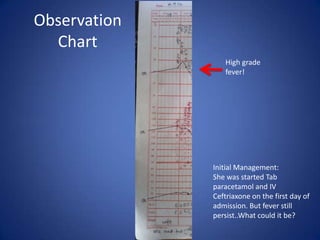
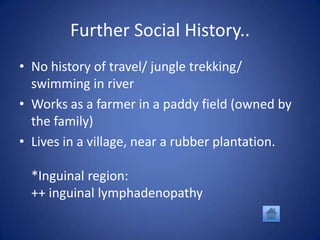
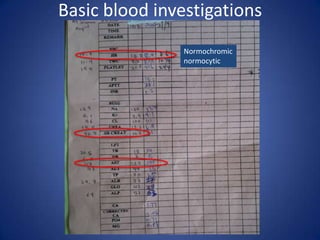
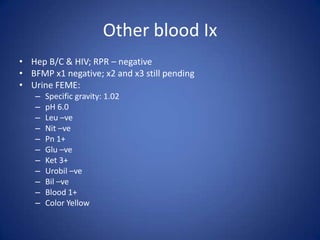
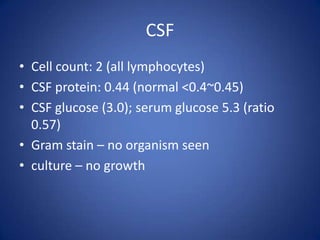
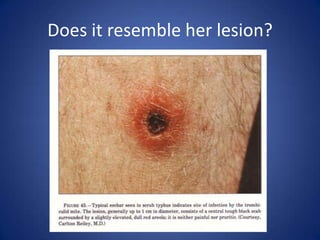
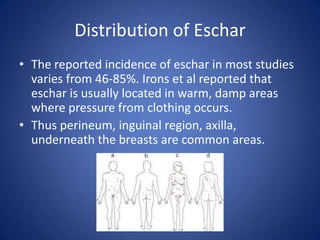
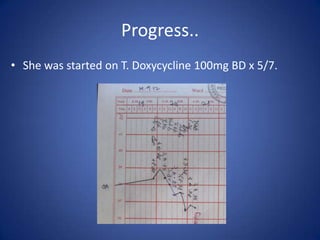
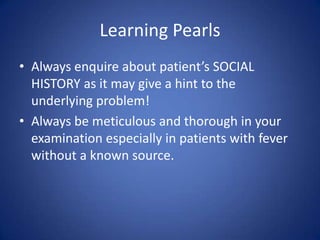
This document describes the case of a 51-year-old female who presented with fever, chills, nausea, and weakness. Initial workup revealed normal vital signs and lab tests. Further examination uncovered an eschar on her abdomen, leading to a diagnosis of scrub typhus. Scrub typhus is an acute febrile illness caused by Orientia tsutsugamuchi transmitted by mites. It is characterized by eschar formation and disseminated rash. The patient was started on doxycycline treatment. Thorough history and examination are important to identify atypical infections like scrub typhus in patients presenting with undifferentiated fever.