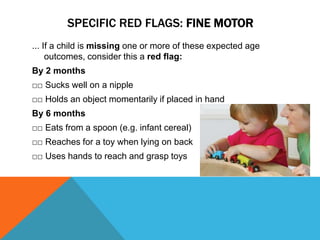
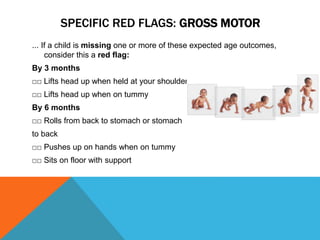
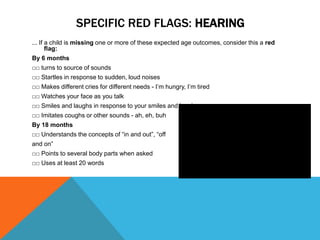
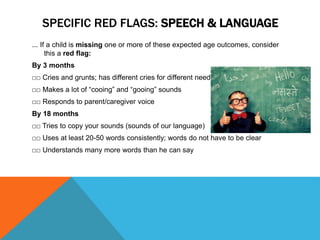
This document provides information about red flags in child development and signs of potential developmental delays or disabilities. It discusses monitoring children's development across physical, cognitive, language, social, and behavioral domains. Parents and caregivers are encouraged to track children's developmental milestones and seek further assessment if milestones are significantly delayed compared to peers. Early intervention can help address delays and improve outcomes for children. The document also provides specific examples of red flags in different developmental areas for various age groups.