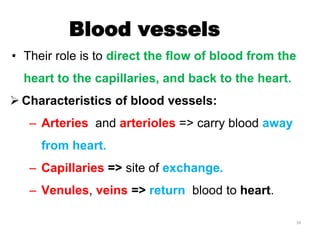
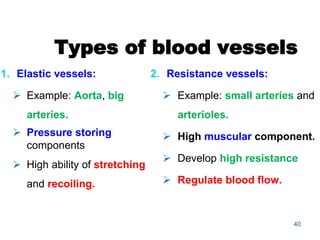
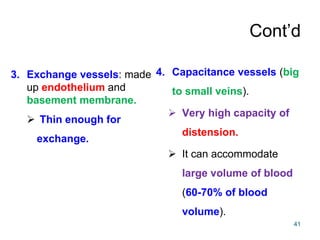
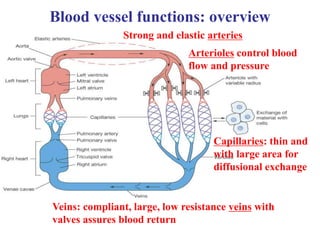
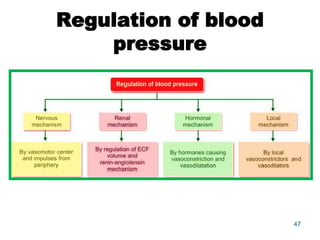
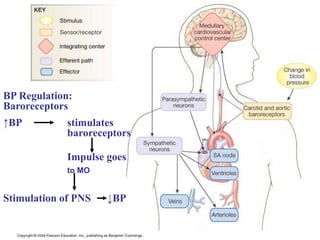
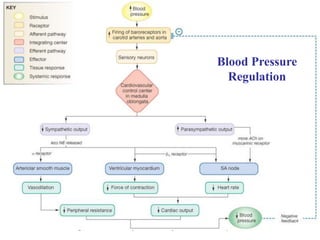
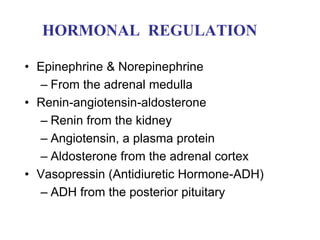
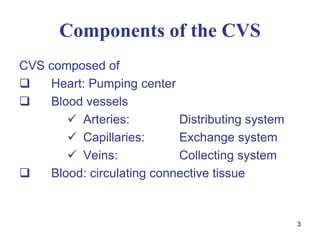
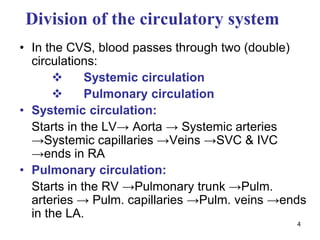
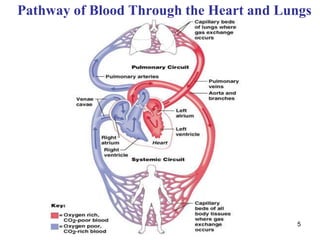
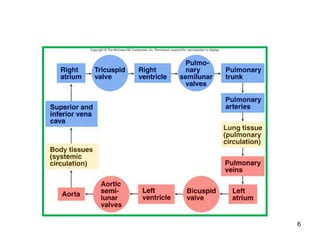
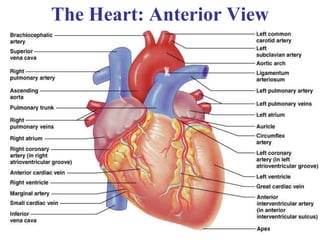
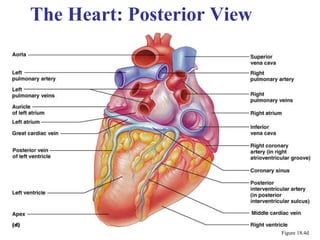
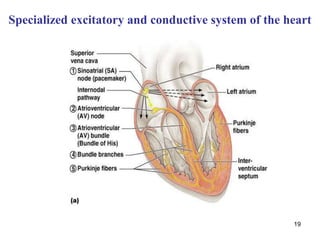
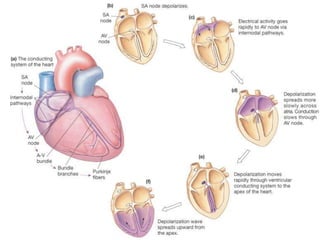
The cardiovascular system functions to transport blood and nutrients throughout the body while removing waste. It is composed of the heart, which pumps blood through a closed system of arteries, capillaries and veins. The heart has four chambers and uses electrical conduction pathways to generate rhythmic contractions. Blood flows through two circuits - systemic circulation which oxygenates tissues, and pulmonary circulation which oxygenates blood in the lungs. The cardiovascular system is regulated through neural and hormonal mechanisms to maintain blood pressure and meet the body's needs.
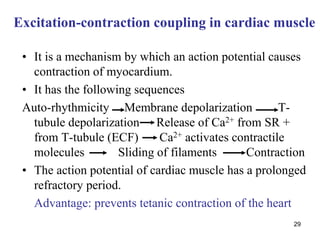
![30
Ca2+
signaling in cardiac muscle
DHPR
(DHPR)
Ca2+
Entry of Ca2+
during
action potential
1 Ca2+
out
for 3 Na+
in
Inhibited by digitalis & ouabain;
indirectly Na+
/Ca2+
exchange
[Ca2+
]in
Affected by epinephrine () and ACh ()](https://image.slidesharecdn.com/chapter5cvsphysiology-1-230301205448-8edc362b/85/chapter_5_CVS_Physiology_-1-ppt-30-320.jpg)