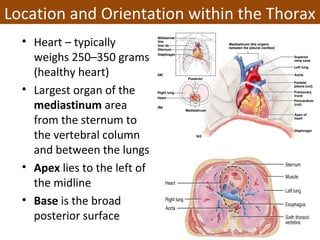
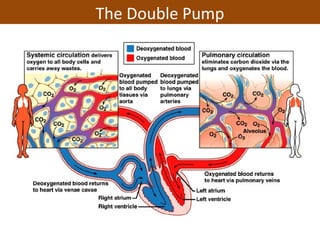
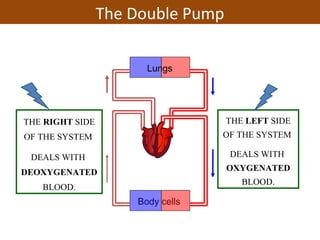
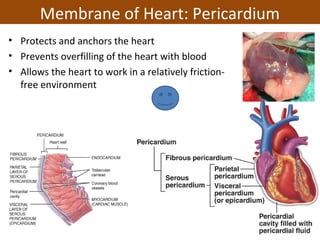
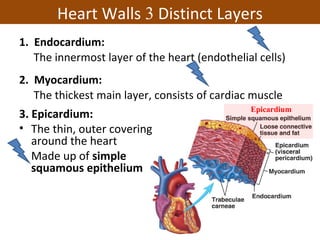
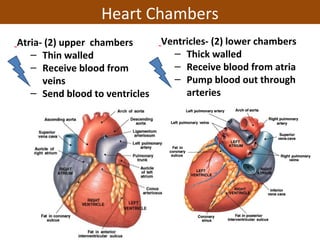
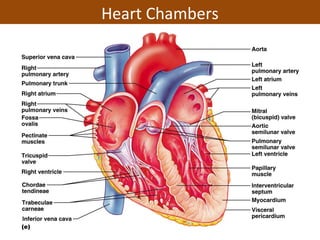
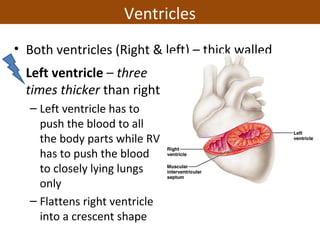
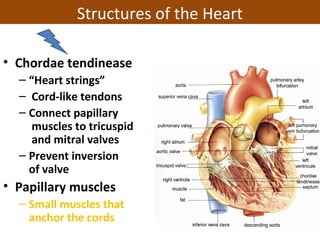
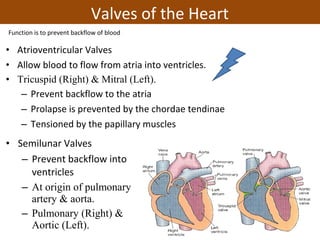
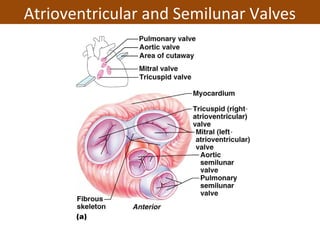
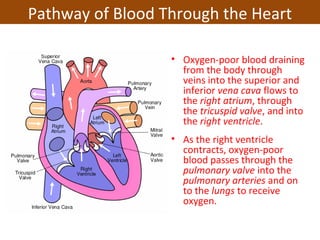
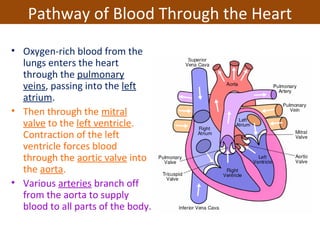
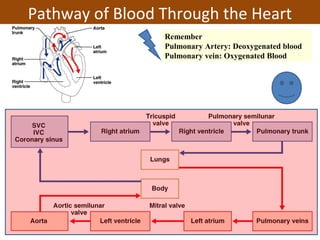
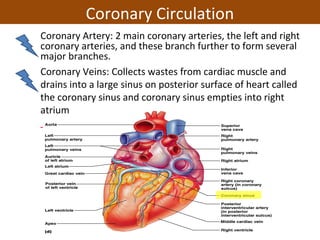
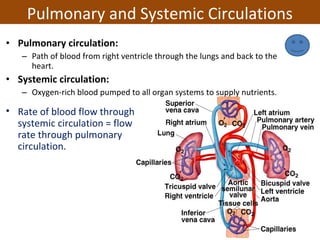
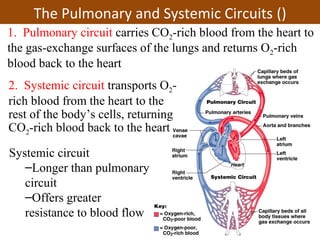
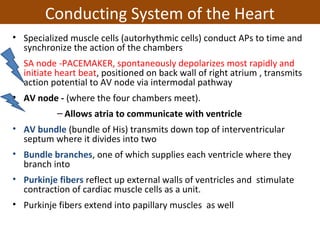
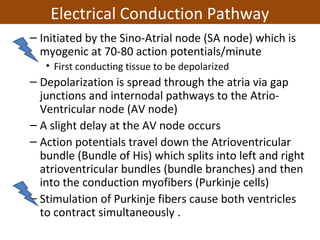
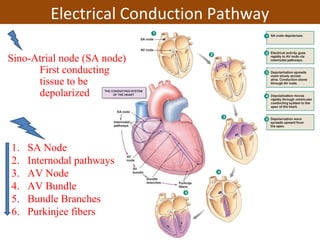
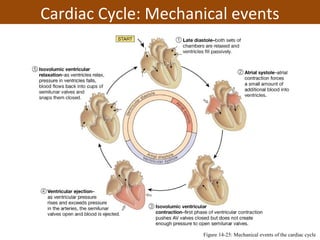
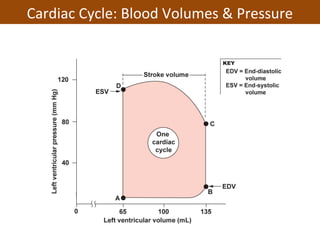
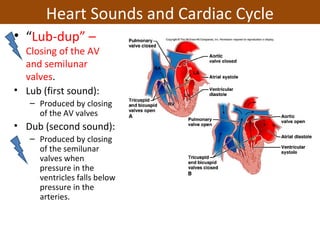
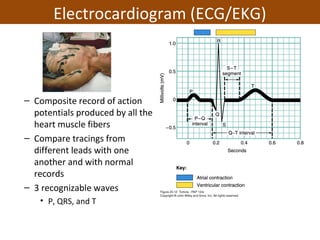
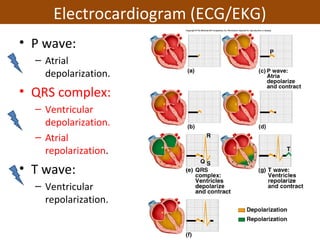
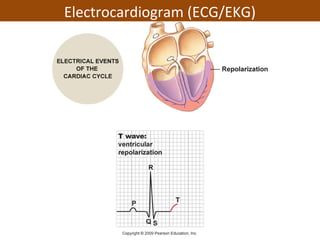
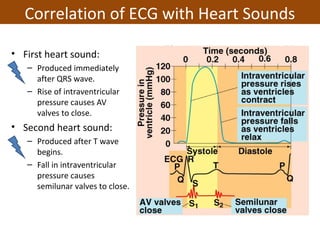
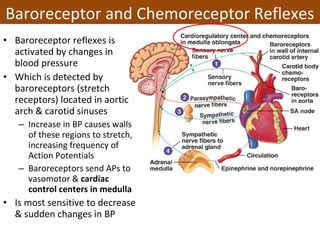
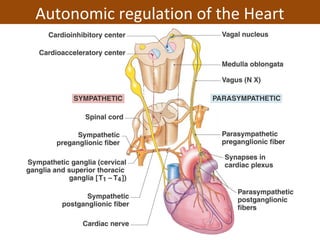
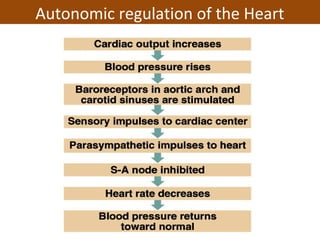
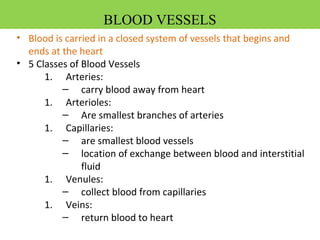
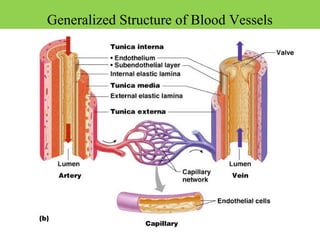
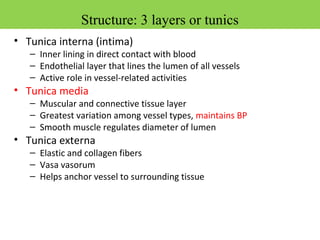
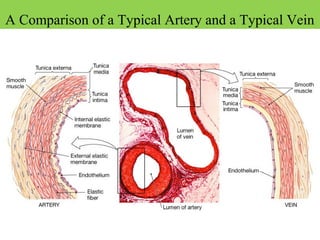
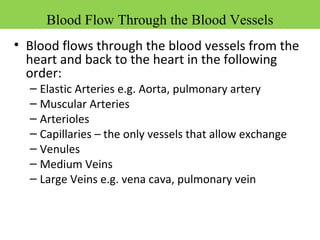
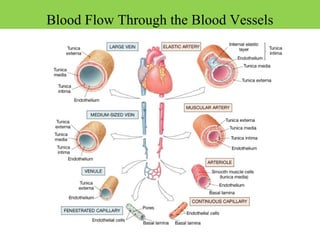
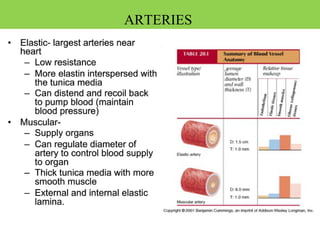
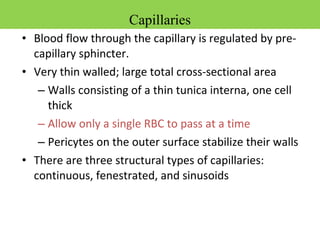
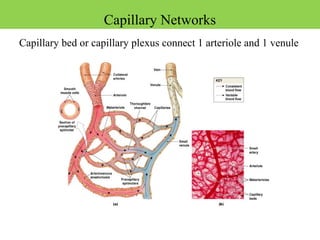
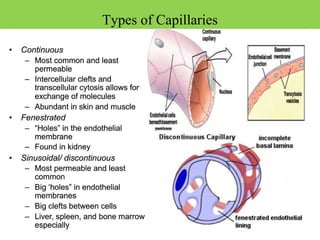
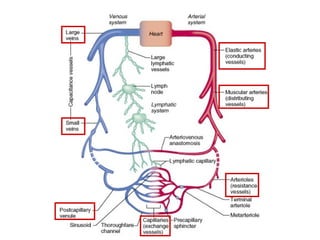
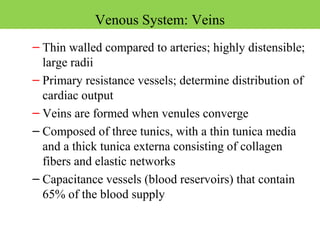
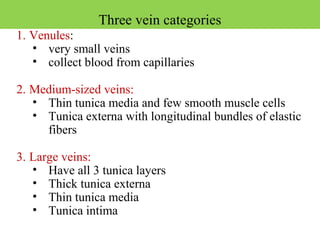
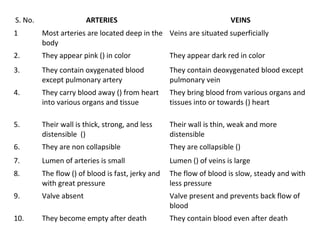
The document provides information about the cardiovascular system and the heart. It discusses the structure and functions of the heart, including the chambers, valves, conduction system, and blood flow pathways. It also covers topics like the cardiac cycle, heart sounds, electrocardiography, regulation of heart rate and blood pressure, and the different types of blood vessels. The heart pumps over 1 million gallons of blood per year to circulate oxygen and nutrients to tissues throughout the body.