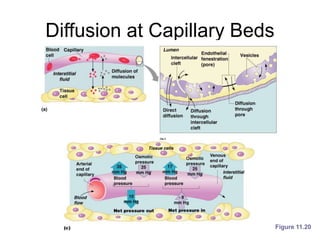
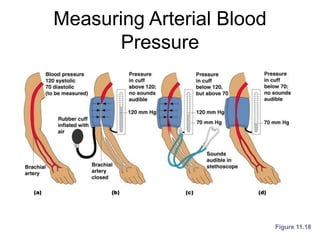
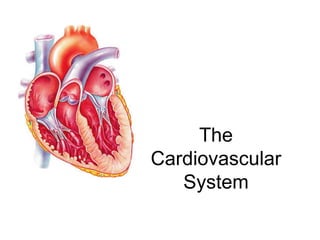
The cardiovascular system consists of the heart and blood vessels. The heart pumps blood through the blood vessels to deliver oxygen and nutrients to tissues and remove waste. It has four chambers - two atria that receive blood and two ventricles that pump blood out. Blood circulates through arteries, capillaries, and veins. In capillaries, oxygen and nutrients diffuse into tissues and carbon dioxide and wastes diffuse into blood. The cardiovascular system maintains blood pressure and blood flow through regulation.









![The Heart: Cardiac Output
• Cardiac output (CO)
– Amount of blood pumped by each side of the
heart in one minute
– CO = (heart rate [HR]) x (stroke volume [SV])
• Stroke volume
– Volume of blood pumped by each ventricle in
one contraction](https://image.slidesharecdn.com/ch11-cardiovascularsystem-210914105745/85/Ch-11-cardiovascular-system-19-320.jpg)