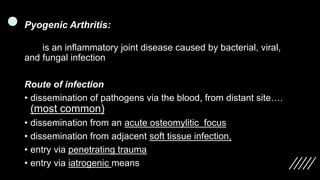
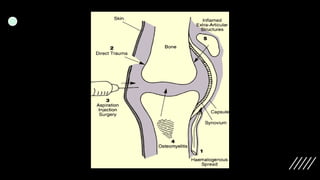
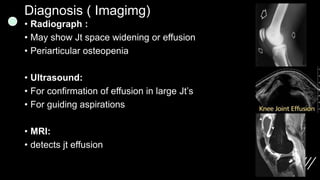
Pyogenic arthritis is an inflammatory joint disease caused by various infections, most commonly from Staphylococcus aureus, and can result from multiple pathways of pathogen entry. Symptoms include fever, joint pain, and swelling, primarily affecting one joint, and diagnosis typically involves imaging and joint fluid analysis. Treatment focuses on joint aspiration, antibiotics, and supportive care to prevent complications like dislocation, growth disturbances, and secondary osteoarthritis.