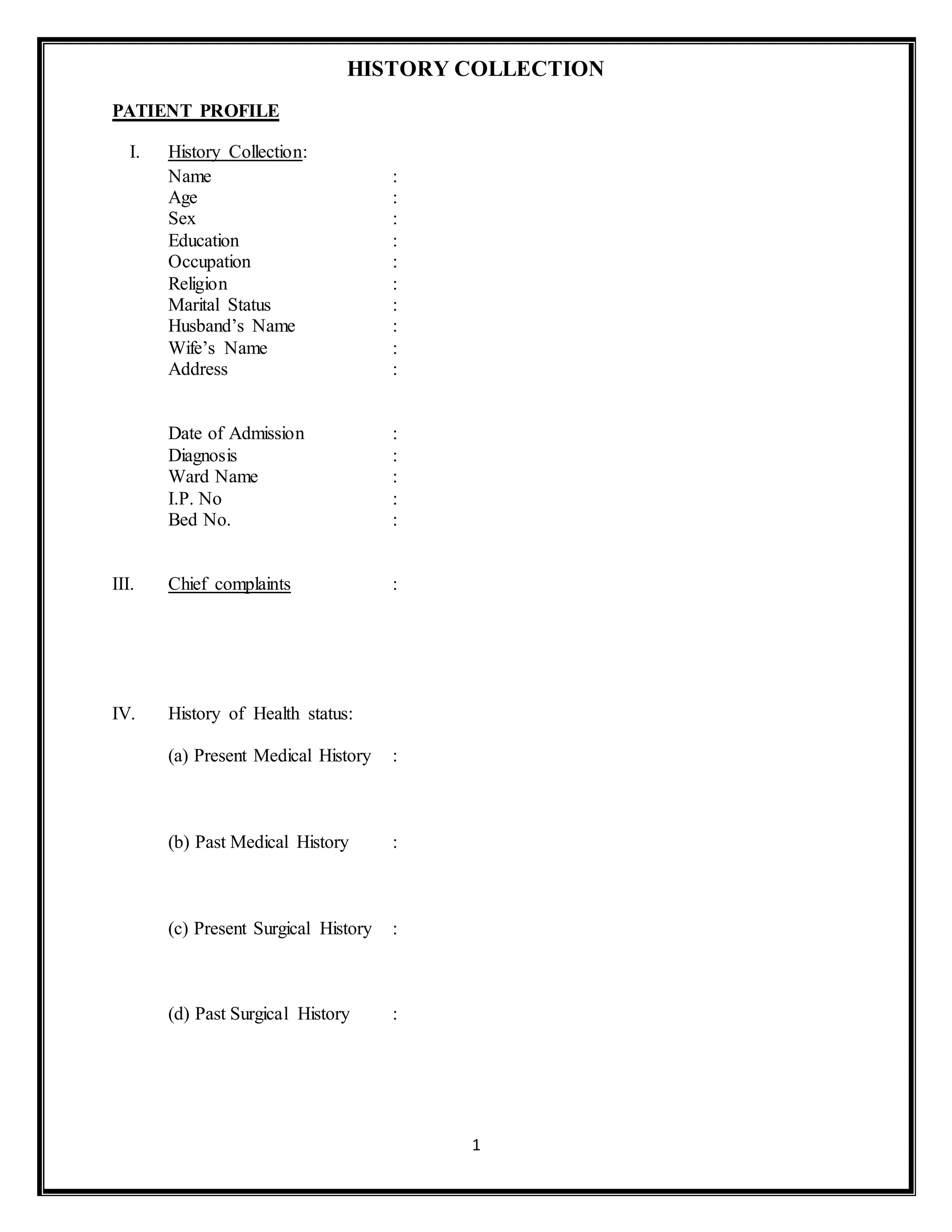
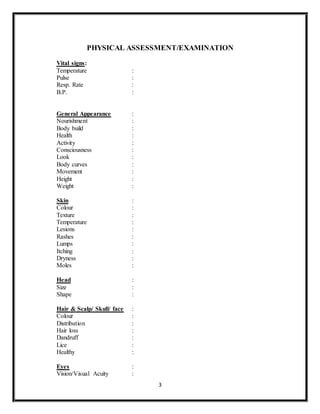
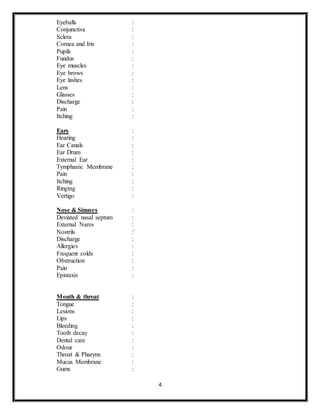
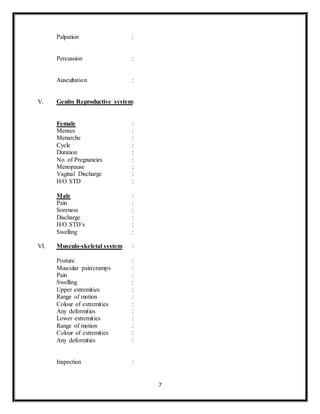
The document outlines a comprehensive patient assessment and care plan, detailing the collection of patient history, physical examinations, diagnostic tests, and nursing responsibilities. It includes sections on vital signs, health status, medical histories, and systematic evaluations across various bodily systems. Additionally, it describes the nursing care plan, discharge planning, and the conclusion reflecting on patient care quality and outcomes.